Impact of Home Visits on Patients with Chronic Disease
Adaptable. Responsive. Equipped with the skills needed to succeed in the future healthcare environment. These are qualities that SOMA graduates learn to apply throughout their careers to meet patient needs in a dynamically changing healthcare environment.
The “1+3” medical school model itself is an example of adaptability that prepares the osteopathic doctors of tomorrow. During the first year, didactic coursework is supplemented with a variety of other innovative methods, such as patient interactions, simulations, medical skills and osteopathic manipulative medicine. The next three years are spent practicing in community clinics, developing a broader understanding of public healthcare through direct interaction with patients.
In this way, SOMA graduates benefit from both traditional learning and an alternative approach that enables them to keep their “pulse” on the healthcare community as it evolves.
Introduction
Specific patient populations, such as those suffering from diabetes or chronic pain, consume a disproportionately large fraction of healthcare resources in our current health care system. Yet, these same populations often experience poor outcomes, personal frustration, and a diminished quality of life as they try to live with their disease. The biopsychosocial aspects of a person’s life must be considered when evaluating and designing treatment plans. The idea of addressing the bio-psycho-social component of an individual’s overall well-being is an area that is unquestionably deficient in our current health care system. Often the person experiencing chronic disease has many concerns aside from their medical issues. In the current health model, the typical physician office visit does not adequately reveal the biopsychosocial dilemmas that often inhibit successful implementation of basic medical advice. It is clear that a shift is needed, in our current practices, if we hope to adequately address the challenges posed by these patient populations. One approach to addressing the complex biopsychosocial interaction includes assessments that are conducted in the home of the individual being treated. The approach provides an intimate analysis of the individual’s real life challenges and opportunities. This project investigates the effectiveness of home visits in exploring the components of a person’s overall well-being with emphasis on the biopsychosocial condition of the person’s life.
Methods
Participant Selection: Participants were selected from amongst the patient population at North County Healthcare in Flagstaff, Arizona. Selection criteria included the following: between 18-64 years old, three or more clinic visits in the last six months, and either a HBA1C greater than nine or a clinical diagnosis of chronic pain.
Study Protocol: The study was divided into three phases.
- Home Visit 1—On the first visit, the World Health Organization (WHO) Quality of Life Survey was administered to each participant to exact a baseline score. In addition to this survey, researchers inquired about other social and psychological factors including social environment, socioeconomic status, health history, social support systems, and barriers to health. After the visit, researchers met with the participants’ primary care provider to discuss findings and a plan of action. The researchers then gathered resources that were to be presented at the next home visit.
- Home Visit 2—Approximately one week after the first visit, the second visit was conducted and findings from the previous visit were presented to participants. Researchers then collaborated with each participant to prepare a tailored health plan.
- Final Phone Interview—After three weeks of implementing the health plan, the researchers re- administered the WHO Quality of Life Survey.
Hypothesis
Conducting in-home assessments using a biopsychosocial model will create greater understanding and a resulting increased effectiveness in patient interventions and outcomes. Improved outcomes will ultimately result in a decreased burden on healthcare systems. Perhaps the most important piece in investigating the biopsychosocial aspects of an individual’s life will be the ability to truly create an improved quality of life.
Data Analysis
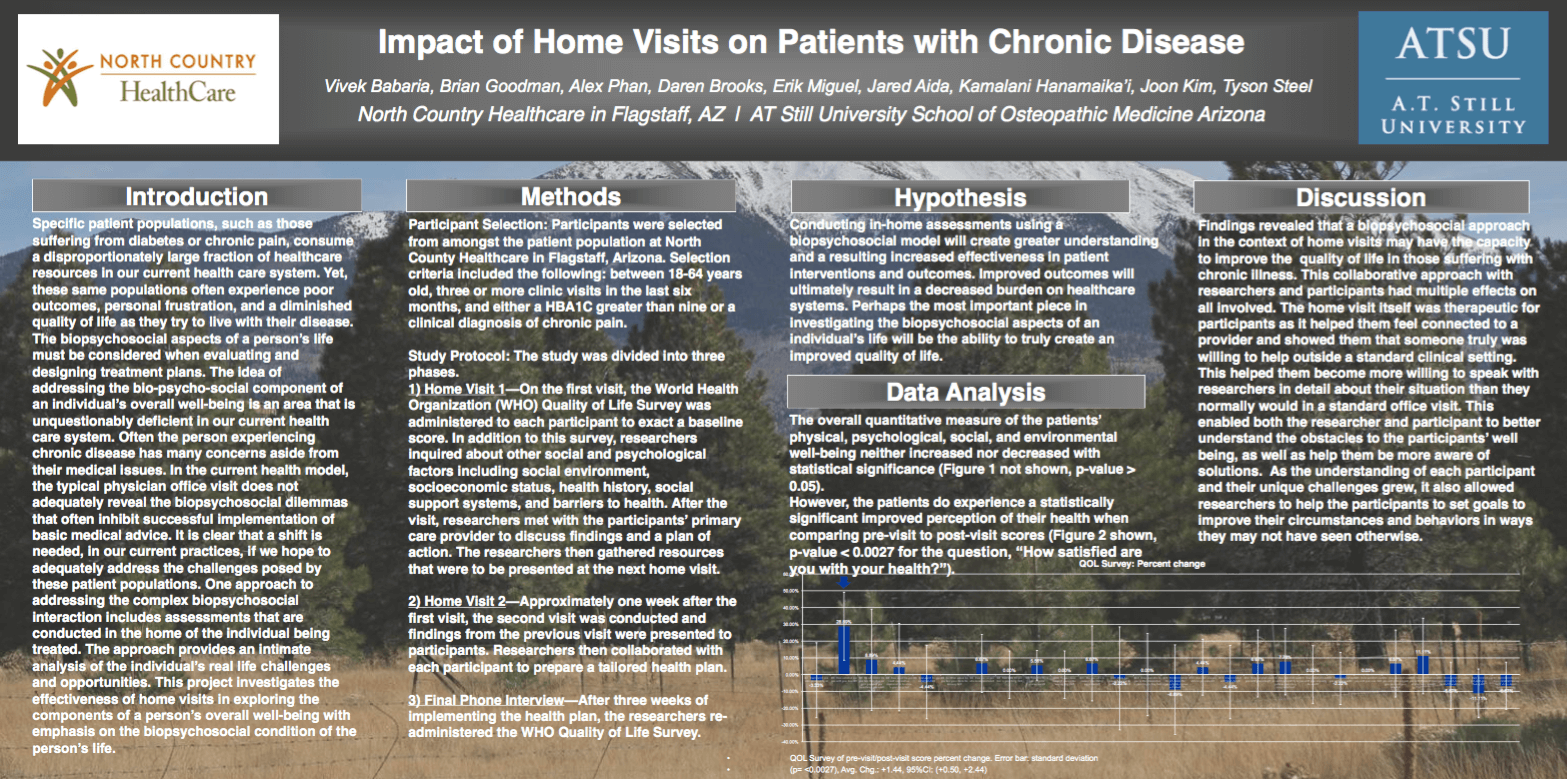
The overall quantitative measure of the patients’ physical, psychological, social, and environmental well-being neither increased nor decreased with statistical significance (Figure 1 not shown, p-value > 0.05). However, the patients do experience a statistically significant improved perception of their health when comparing pre-visit to post-visit scores
Discussion
Findings revealed that a biopsychosocial approach in the context of home visits may have the capacity to improve the quality of life in those suffering with chronic illness. This collaborative approach with researchers and participants had multiple effects on all involved. The home visit itself was therapeutic for participants as it helped them feel connected to a provider and showed them that someone truly was willing to help outside a standard clinical setting. This helped them become more willing to speak with researchers in detail about their situation than they normally would in a standard office visit. This enabled both the researcher and participant to better understand the obstacles to the participants’ well being, as well as help them be more aware of solutions. As the understanding of each participant and their unique challenges grew, it also allowed researchers to help the participants to set goals to improve their circumstances and behaviors in ways they may not have seen otherwise.