Evaluating a Decreased Vaccination Compliance Rate
among Patients Less than Two Years of Age
SOMA graduates enter residency with a greater degree of comfort and preparedness due to the school’s exceptional curriculum structure. As a result, SOMA graduates tend to score higher when rated by their residency directors.
SOMA’s unique Clinical Presentation Curriculum Model is based on the various ways patients present to physicians. Collectively, the clinical presentations represent common patient complaints (e.g., headache, abdominal pain), abnormalities of physical examination (e.g., systolic heart murmur), or abnormalities of commonly ordered laboratory studies, (e.g., anemia, hypocalcemia). Altogether, there are approximately 120 presentations that comprise the SOMA curriculum. The presentations serve as a starting point for the generation of relevant curricular content. This learning approach provides a lasting foundation of knowledge that informs residencies and results in higher ratings.
INTRODUCTION
To address the significant shortage of primary care physicians, we sought to:
- The Lutheran Family Health Center’s (LFHC) Network relies on the Center for Disease Control’s (CDC) Vaccines For Children (VFC) Program to accommodate their patient populations’ vaccination needs.
- In the past year, the LFHC Network lost a portion of their vaccination allocation from the VFC Program due to a 6% decrease in their vaccination compliance rate among patients under two years of age. Six percent decrease was determined by Lutheran’s Internal Quality Assurance Office.
OBJECTIVES
- The aim of this quality assessment project was to determine if the 6% decrease in vaccination compliance among patients less than two was due to provider- controlled lost opportunity for vaccination, a situation when a provider interacts with a child who could be immunized and does not recommend or order necessary immunizations for that child.
METHODS
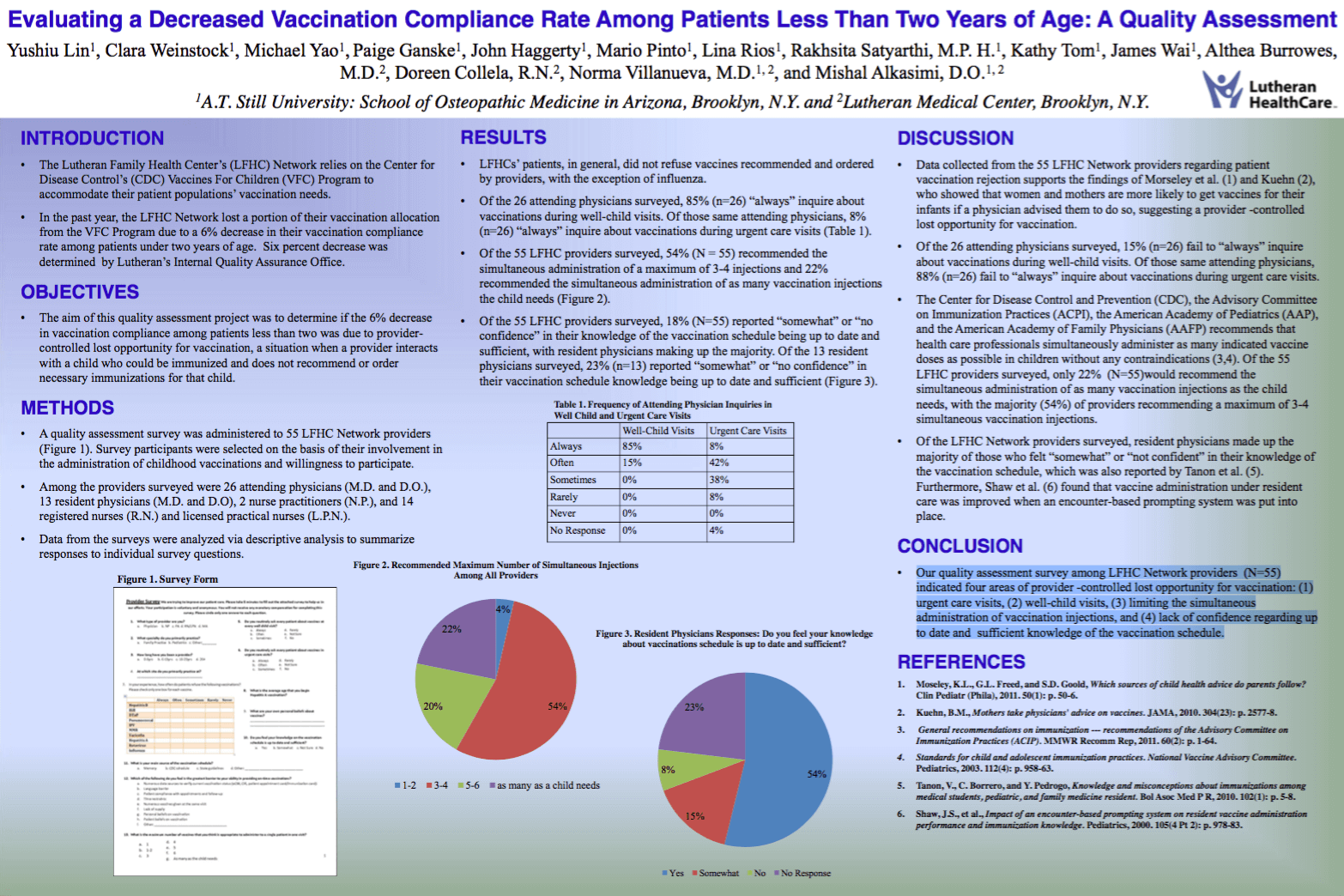
- A quality assessment survey was administered to 55 LFHC Network providers (Figure 1). Survey participants were selected on the basis of their involvement in the administration of childhood vaccinations and willingness to participate.
- Among the providers surveyed were 26 attending physicians (M.D. and D.O.), 13 resident physicians (M.D. and D.O), 2 nurse practitioners (N.P.), and 14 registered nurses (R.N.) and licensed practical nurses (L.P.N.).
- Data from the surveys were analyzed via descriptive analysis to summarize responses to individual survey questions.
RESULTS
- LFHCs’ patients, in general, did not refuse vaccines recommended and ordered • by providers, with the exception of influenza.
- Of the 26 attending physicians surveyed, 85% (n=26) “always” inquire about vaccinations during well-child visits. Of those same attending physicians, 8% (n=26) “always” inquire about vaccinations during urgent care visits (Table 1).
- Of the 55 LFHC providers surveyed, 54% (N = 55) recommended the • simultaneous administration of a maximum of 3-4 injections and 22% recommended the simultaneous administration of as many vaccination injections the child needs (Figure 2).
- Of the 55 LFHC providers surveyed, 18% (N=55) reported “somewhat” or “no confidence” in their knowledge of the vaccination schedule being up to date and sufficient, with resident physicians making up the majority. Of the 13 resident physicians surveyed, 23% (n=13) reported “somewhat” or “no confidence” in their vaccination schedule knowledge being up to date and sufficient (Figure 3).
DISCUSSION
To address the significant shortage of primary care physicians, we sought to:
- Data collected from the 55 LFHC Network providers regarding patient vaccination rejection supports the findings of Morseley et al. (1) and Kuehn (2), who showed that women and mothers are more likely to get vaccines for their infants if a physician advised them to do so, suggesting a provider -controlled lost opportunity for vaccination.
- Of the 26 attending physicians surveyed, 15% (n=26) fail to “always” inquire about vaccinations during well-child visits. Of those same attending physicians, 88% (n=26) fail to “always” inquire about vaccinations during urgent care visits.
- The Center for Disease Control and Prevention (CDC), the Advisory Committee on Immunization Practices (ACPI), the American Academy of Pediatrics (AAP), and the American Academy of Family Physicians (AAFP) recommends that health care professionals simultaneously administer as many indicated vaccine doses as possible in children without any contraindications (3,4). Of the 55 LFHC providers surveyed, only 22% (N=55)would recommend the simultaneous administration of as many vaccination injections as the child needs, with the majority (54%) of providers recommending a maximum of 3-4 simultaneous vaccination injections.
- Of the LFHC Network providers surveyed, resident physicians made up the majority of those who felt “somewhat” or “not confident” in their knowledge of the vaccination schedule, which was also reported by Tanon et al. (5). Furthermore, Shaw et al. (6) found that vaccine administration under resident care was improved when an encounter-based prompting system was put into place.
CONCLUSION
Our quality assessment survey among LFHC Network providers (N=55) indicated four areas of provider -controlled lost opportunity for vaccination: (1) urgent care visits, (2) well-child visits, (3) limiting the simultaneous administration of vaccination injections, and (4) lack of confidence regarding up to date and sufficient knowledge of the vaccination schedule.