New Interprofessional Cross-Campus Collaborative Case coming Summer 2026!

Your team task
Your team is about to take over the care of Bobby Walker, who was seen in the Emergency Department. He presented with shortness of breath, pain and swelling of the left wrist and decreased grip strength due to pain following a fall caused by shortness of breath that occurred during a training run for a “Couch to 5K” program. He also suffered a mouth injury in the fall. He was diagnosed with left comminuted and angulated distal radial fracture (colles), left ulnar styloid fracture, lip laceration, dental fractures 2° to fall, and Obstructive Pulmonary Disease. Concerns about hearing were also noted during this time.
You are provided with the following information to help you with your task.
- Audio and written narratives from patient Bobby Walker, Wife Brianne Walker, and Bobby’s daughter-in-law Ella Walker.
- A description of Bobby Walker’s hometown.
- Documentation from the health professions involved in Bobby’s care during his Emergency Department visit and subsequent follow up care.
Your team is tasked with:
- Identifying the holistic needs of Bobby Walker and his family.
- Building an interprofessional team with the skills to meet the needs of Bobby Walker and his family
As you work together to build the team to care for Bobby Walker and his family you must consider:
- The holistic needs of Bobby Walker and his family.
- How you can place the interests of Bobby and his family at the center of the interprofessional team.
- The composition of the interprofessional team, identifying the roles and responsibilities of those involved and how they relate to the identified needs for this family.
- Specific team strategies you will use to ensure the interprofessional team functions as an effective team.
- Specific communication strategies the team will use to ensure they practice effective interprofessional communication.
- How quality improvement and patient safety will be addressed by the team.
The core competencies for interprofessional collaboration
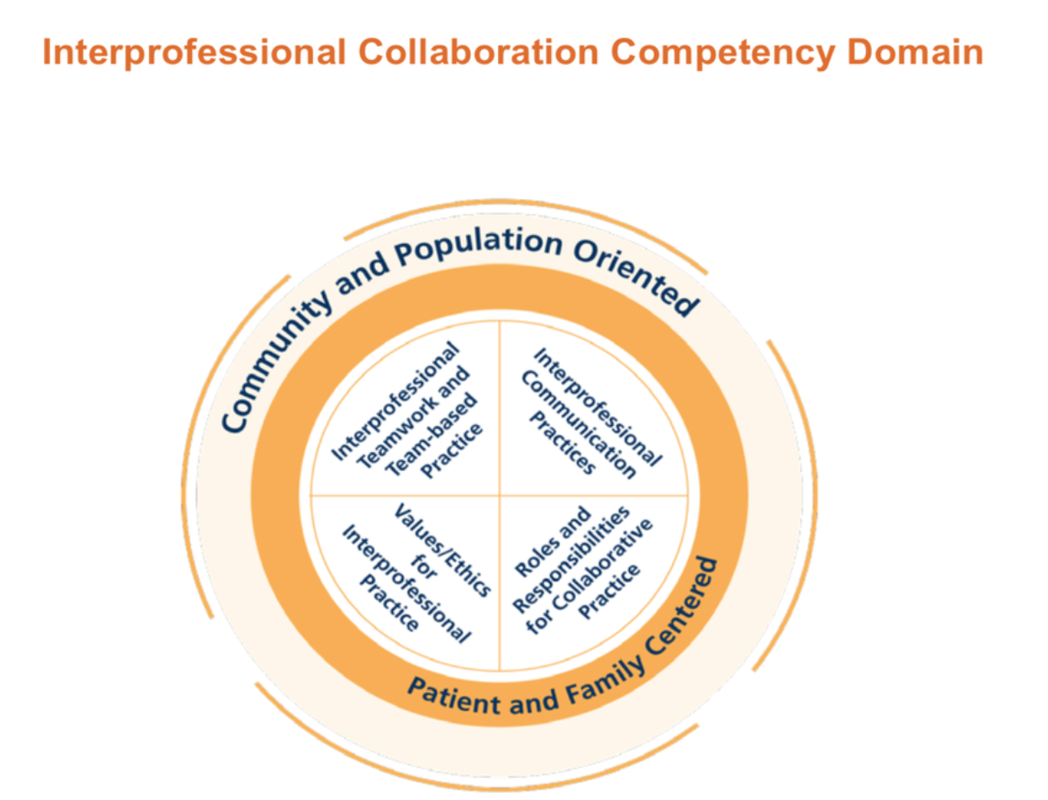
Use the 4 core competencies for interprofessional collaborative practice to guide you on the issues to consider:
- Work with individuals of other professions to maintain a climate of mutual respect and shared values. (Values/Ethics for Interprofessional Practice)
- Use the knowledge of one’s own role and those of other professions to appropriately assess and address the health care needs of patients and to promote and advance the health of populations. (Roles/Responsibilities)
- Communicate with patients, families, communities, and professionals in health and other fields in a responsive and responsible manner that supports a team approach to the promotion and maintenance of health and the prevention and treatment of disease. (Interprofessional Communication)
- Apply relationship-building values and the principles of team dynamics to perform effectively in different team roles to plan, deliver, and evaluate patient/population-centered care and population health programs and policies that are safe, timely, efficient, effective, and equitable. (Teams and Teamwork)

Teams
Once you register for the collaborative event, you will be placed into a small interprofessional team and will be assigned a team facilitator. Names and contact information for your teammates and facilitator will be sent to you prior to orientation. By the end of the orientation event, your team should have developed a plan as to how you will communicate and function to complete the assigned tasks.
Interaction with facilitators
A faculty team facilitator will be assigned to each team. The faculty team members who developed the case will serve as facilitators for your group and can help guide you through the task. So please feel free to ask for help in understanding the assigned task. Your facilitator is able to:
- Provide feedback/guidance to your team as you work through the case and prepare your presentation.
- Review your plan/presentation prior to your final team presentation.
- Provide feedback and comments during your practice session.
The presentations
Your end product is an oral presentation, presented via Zoom, which demonstrates your reflection on the life story and care of Bobby Walker and his family, and the professionals you would include in an interprofessional team to meet their needs.
You are also asked to provide a short reflective piece in your presentation on your own team's experience of collaboration in action, including what you have learned about the other professions' roles and responsibilities, team working, and communication issues.
Presentation structure
Each team will have 20 minutes to present their work. A 5-minute, 3-minute and 1-minute warning will be given to the team. At the conclusion of 20 minutes, the timekeeper will announce time and your team must stop their presentation. No team will be permitted to exceed the allocated 20-minute time limit. If the team completes its presentation prior to the 20-minute time limit, the team should announce that they have completed their presentation. Presentations will be followed by a 10-minute question and answer period with a panel of judges.
Each team member must participate equally in both the oral presentation and the question and answer period immediately following the team presentation.
Teams are encouraged to invite friends and other students to attend their presentation. By the time of your scheduled rehearsal, please let your facilitator know the names and email addresses of any people you would like to invite. The audience may include other non-participating students, faculty, and interested health professionals. Audience members are requested not to ask questions or use the chat feature during the presentations.
Judges will complete a scoring sheet for each team presentation. An average score will be calculated for each team. Teams will be provided with their team score and feedback after the event.
Grading Rubric (download)

About Bobby Walker
Bobby Walker is 41 years old and lives in Decatur, Illinois. He works as a railroad engineer and enjoys attending truck and tractor pulls. Previously a life-long smoker, Bobby quit smoking and took up chewing tobacco when his son died in 2024 during an Army training session in a helicopter. Bobby has recently begun training for a Couch to 5K to honor his son’s memory. Recently while on a training run, Bobby, with a history of asthma, became short of breath and fell. Bobby was seen in the Emergency Department and presented with shortness of breath, pain and swelling of the left wrist and decreased grip strength due to pain from the fall. He also suffered a mouth injury in the fall. He was diagnosed with left comminuted and angulated distal radial fracture (colles), left ulnar styloid fracture, lip laceration, dental fractures 2° to fall, and Obstructive Pulmonary Disease. Concerns about hearing were also noted during this time.
Listen to Bobby’s Emergency Department narrative (audio file)
Read Bobby’s Emergency Department narrative (pdf)
Listen to Bobby’s Follow Up narrative (audio file)
Read Bobby’s Follow Up narrative (pdf)
Listen to Bobby’s wife’s narrative (audio file)
Read Bobby’s wife’s narrative (PDF)
Listen to Bobby’s daughter-in-law’s narrative (audio file)
Read Bobby’s daughter-in-law’s narrative (PDF)
Bobby’s home town of Decatur, Illinois
General City Information: Decatur is located in Macon county in central Illinois. Decatur was founded in 1829 along the Sangamon River and Lake Decatur, and as of 2020 is the largest city in Macon county with a population of 70,522 people. It is the sixth most populous city in Illinois outside the Chicago metropolitan area and its economy is based on industrial and agricultural commodity processing and production. Decatur houses production facilities for Caterpillar, Archer Daniels Midland, Mueller Company and Primient.1Abraham Lincoln’s first Illinois home was in Decatur. Lincoln argued 5 cases as a lawyer in the log courthouse that now resides on the grounds of the Macon County Historical Museum. For much of the 20th century, Decatur was known as “The Soybean Capital of the World.1
Decatur is home to two public high schools and seven public elementary schools.2
Decatur Area Healthcare: Decatur is home to HSHS St. Mary’s Hospital, a 144-bed hospital and provides "specialty services in cardiac care, surgery, medical imaging, laboratory, emergency medicine”3 among others. Also, Decatur Memorial Hospital is a 280-bed hospital that is a designated Level II Trauma Center and a Primary Stroke Center, with inpatient services such as orthopedics, cardiopulmonary, vascular medicine, gastroenterology, oncology, emergency medicine, laboratory and radiology services. Their outpatient services include infusion, physical therapy, and cancer care, among others.4
Economics: “The cost of living in Decatur, IL is 20.6% lower than the national average.”5 The living wage for a household of two (but with only one adult working) is $59,300.80 annually.6
Sources:
1 Wikipedia
2 Decatur Public Schools
3 HSHS St. Mary’s Hospital
4 Decatur Memorial Hospital
5 apartments.com
6 Living Wage Calculator
Bobby Walker’s emergency department visit
Bobby Walker presented at the Emergency Department with shortness of breath, pain and swelling of the left wrist and decreased grip strength due to pain following a fall caused by shortness of breath that occurred during a training run for a “Couch to 5K” program. He also suffered a mouth injury in the fall. He was diagnosed with left comminuted and angulated distal radial fracture (colles), left ulnar styloid fracture, lip laceration, dental fractures 2° to fall, and Obstructive Pulmonary Disease. Concerns about hearing were also noted during this time.Physician/PA Urgent Care Note
EMERGENCY ROOM NOTE (PA)
Patient Demographics:
Patient Name: Walker, Bobby DOB: 07/04/1984 Age: 41 years old
Ethnicity:
Caucasian
Insurance: Insured
Health Care Setting: Decatur Memorial Hospital:
Emergency Department
Chief Concern: Fall, shortness of breath, left wrist pain, mouth injury X today.
Vitals:
Ht: 6'2"; Wt: 210 lbs; BP: 147/95 mmHg; HR: 84bpm;
RR: 16 bpm; Temp: 98.7 F (oral); O2 Sat: 98% RA
Subjective:
Mr. Bobby Walker is a 41-year-old male who presents to the Emergency
Department following a fall that occurred during a training run for a "Couch to 5K" program. While
running, he became short of breath and reports the shortness of breath as the cause of his fall. He
reports chronic shortness of breath which worsened with exertion. He denies any chest pain, sweating,
nausea, vomiting. Upon impact, his head struck the ground, resulting in injuries to his tooth, lip, and
gums. He injured his left wrist. He reports no loss of consciousness. Prior to this event, he was
participating in a "Couch to 5K" training program. Last Tdap was > 10 years ago. Current pain level is
8/10. Patient is left-handed. Is employed as a railroad engineer.
ROS:
General: Denies fever, chill, malaise.
Neuro / Head: Mild headache.
Denies LOC or confusion.
Neck: Denies neck pain. Denies UE numbness /
tingling.
EENT: Reports lip laceration and associated pain along with dental injuries and
associated pain.
Resp: Positive for shortness of breath and a dry cough. Denies sputum
production.
Cardio: Denies chest pain, palpitations, sweats, nausea or
vomiting.
Abdomen Denies abdominal pain, nausea, vomiting or changes to bowel
habits.
Extremities: Admits to pain and swelling of left wrist and decreased grip strength due
to pain. Denies numbness / tingling.
Objective:
General: Spouse is present with the patient in the room during the
encounter. Patient appears to be in moderate acute distress from pain and shortness of breath and
requests some questions to be repeated several times during the encounter due to not being able to hear
well while in the noisy ED.
Head / Eyes / Ears / Nose / Throat (HEENT): Head: Normocephalic
without evidence of trauma to the scalp. Eyes: Pupils Equal Round Reactive to Light and
Accommodates (PERRLA) bilaterally. Ears: No evidence of trauma. Tympanic membranes are
intact atraumatic, pearly grey with intact light reflex. Oral: Laceration noted to the lip.
Gingiva edematous and bleeding present suspect associated dental fractures. TMJ:
non-tender to palpation, full range of motion (FROM) with 3 finger horizontal width between front teeth
when mouth is open, able to clench and slide without difficulty.
Cardiac: No evidence of chest wall trauma. Regular rate and rhythm (RRR) without murmurs, gallops, rubs.
Respirations: Chest wall is atraumatic, non-tender to palpate, no flail chest present. Lungs are clear to auscultation with decreased sounds at the bases bilaterally.
Abdomen: Atraumatic. Bowel sounds are present in all 4 quadrants and non-distended, non-tender to palpation. No organomegaly.
Extremities: Left wrist: moderately edematous, early ecchymosis present, fork deformity of the distal radius suggesting fracture, is tender to palpate with decreased range of motion with 0° flexion and extension due to pain. Left Hand: positive for superficial abrasion to the volar aspect specifically at the thenar eminence, mild edema present, full active and passive range of motion of all fingers and distal neurovascularly intact with capillary refill at less than 2 seconds and radial and ulnar pulses palpable. Left elbow: atraumatic, nontender to palpation, full active and passive range of motion. Right upper extremity: atraumatic, non-tender to palpation, full active and passive range of motion present. Lower extremities: atraumatic and non-tender to palpation, full range of motion active and passive intact.
Neurological: Cranial Nerves 2 through 12 are intact. Ambulation and gait is stable.
Orders:
- CT Scan: skull, facial, brain w/o contrast
- CT Chest w/o contrast
- Xray: Left wrist 3 views: PA / Lateral /Oblique and Navicular
- IV placement
- Morphine sulfate 10mg IV push
- Ondansetron 8 mg IV push
- Tdap immunization
Consultation: Spoke with Dr. Justine Matinez, who is the on-call orthopedist, and advised in-ED closed reduction to improve alignment prior to splinting and ortho follow-up.
Procedure Note:
Verbal and written consent is obtained from the patient after risks, benefits,
alternatives were discussed and all questions answered regarding left wrist closed reduction under
sedation. The patient is placed on a cardiac monitor and is adequately sedated using midazolam 5mg IV
with respiratory therapy providing oxygen and respiratory monitoring. Reduction of the displaced
fracture was successful as evidenced with post-reduction films. The patient remains neurovascularly
intact and a long arm sugar tong with thumb spica is placed by me with the assistance of the medical
technician.
Reassessment: 60 minutes after the morphine, patient was reassessed and appears more comfortable. Patient reports the pain to be 4/10 now. Otherwise the physical exam remains unchanged.
Assessment:
- Fall, unintended, non-syncopal
- Left comminuted and angulated distal radial fracture (colles); closed reduction successful
- Left ulnar styloid fracture; stable
- Lip laceration - not requiring primary closure repair
- Dental fractures 2° to fall
- Shortness of breath; acute exacerbation of chronic
- Chronic Obstructive Pulmonary Disease
- Decreased hearing acuity
Plan:
- Left orthoglass splint: long arm sugar-tong with thumb spica applied and distal neuro-vasc checked and intact after placement.
- Hydrocodone 5/325: 1 - 2 PO Q 6 hours as needed for severe pain #20 x No refills
- OTC Ibuprofen 400mg Q 8 hours for pain not to exceed 2 weeks use
- Follow up with your Primary Care Provider within 3 days for re-check and further care.
- Follow up with your dentist within 3 days.
- Wrist fracture care discussed and patient verbalized understanding.
- Dental fracture care discussed.
- Lip laceration care discussed.
- Return to the ED if any symptoms worsen such as increased pain, numbness / tingling of the hand.
- Return to the ED or call 911 if worsening shortness of breath or chest pain.
Medical Decision Making: All questions were answered from the patient and his spouse. Patient is alert and oriented and able to make medical decisions. Patient is stable and there are no neurovascular emergencies at this time related to the fracture. No evidence of intracranial emergency at this time.
Electronically Signed:
Jacqualine Dancy, MPAS, PA-C; Supervising physician: Dawn Waters, DO
Left Wrist Xray: (Colles Fracture Distal Radius)

Radiology report:
Patient Name: Walker, Bobby; DOB: 07/04/1984; Age: 41
years old
Indications: Fall with left wrist pain.
Technique: Standard radiographic series of the left wrist was performed, including PA, Lateral, and Oblique and scaphoid views.
Bones: There is an acute, comminuted, fracture of the distal left radius with significant dorsal angulation and dorsal displacement of the distal radial fragment are noted, characteristic of a Colles fracture. An associated fracture of the ulnar styloid process is identified. Scaphoid intact without fractures. The radiocarpal joint space is preserved.
Soft Tissues: Swelling of the soft tissues surrounding the wrist is present. No significant soft tissue foreign bodies or air are seen.
Impression:
- Acute left distal radius fracture dorsally angulated, comminuted with surrounding soft tissue swelling
- Acute left ulnar styloid fracture
Recommend: Correlate findings clinically. CT scan or MRI as clinically indicated.
Electronically Signed: Elijah Bainbridge, DO
Post-Reduction Film:

Radiology report:
Patient Name: Walker, Bobby; DOB: 07/04/1984; Age: 41
years old
Indication: Post-reduction left wrist
Impression:
Improved position of the distal radius fragment indicating successful reduction. Of
note, the radiograph is taken while the patient is in splint to preserve the position of the reduction.
Electronically Signed: Elijah Bainbridge, DO
Athletic Trainer Notes
Athletic Training Notes
Walker, Bobby
Subjective:
- 41-year old male went to ED
- Fall during training for “Couch to 5K” run
- While running had shortness of breath – said that was reason for fall
- Reports chronic shortness of breath – worsens with exertion
- No chest pain, sweating, nausea, vomiting
- When fell – head hit ground, visual injury to tooth, lip, and gums
- L wrist has pain
- No LOC
- Pain is 8/10
- Left-handed
- Employed as railroad engineer
- Complains of mild headache
- No confusion
- No neck pain
- Complains of lip pain and pain with dental injuries
- Has a dry cough
- No abdominal pain
- Pain in L wrist and decreased grip strength due to pain
Objective
- Observe lip laceration
- Observe moderate pain and shortness of breath when answering questions
- Has to have questions repeated due to not being able to hear with background noise
- (-) concussion tests/assessments
- (-) anterograde and retrograde amnesia
- PEARL equal bilaterally
-
Left Wrist
- Decreased AROM bilaterally of finger flexion (making a fist), pain noted with RROM with finger flexion
- Capillary refill equal bilaterally
- Radial and ulnar pulses palpable
- Full AROM and PROM bilaterally of elbow flexion and extension
- Full AROM and PROM bilaterally of shoulder movements
- Pain noted with L wrist flexion/extension, decreased AROM bilaterally
- Pain noted and unable to supinate and pronate L wrist with AROM
- Dental
- Observe tooth displaced
Assessment
- Tuning fork caused pain on distal radius
- Pain with resisted supination/pronation
- Pain with squeeze test
- Weakness noted with finger abduction
Plan
- Refer for X-Ray for L wrist
- Refer for imaging of head
- Patient education for concussion
- Lip laceration care and patient education
- Ice
- Refer to orthopedic for wrist
- Rehabilitation plan for L wrist
- Discuss plan for training for 5K safely – develop plan
Audiology Note
Audiology Note
Patient Name: Bobby Walker
DOB: 07/04/1984
Date: xx/xx/2025
S: Bobby Walker was referred for an audiologic evaluation following a recent emergency room visit. He was alert and cooperative throughout the evaluation and provided his own case history information. Mr. Walker reported occasional difficulty hearing, which seems to have worsened over the years. He reported particular concern about his ability to hear during interactions with health care providers, particularly surrounding his recent COPD diagnosis. He indicated that he recently misunderstood what a health care provider was asking him and he was concerned that he would miss important questions or instructions surrounding his treatment. He reported interest in learning more about hearing aids if they are indicated for him. He reported a history of some noise exposure through various noisy jobs throughout his life (farm work, primarily) and attending loud concerts. He denied a history of hearing aid use. He reported intermittent tinnitus at both ears. He denied a history of vertigo. He denied a history of aural pain, fullness, pressure, or drainage. He denied a history of hypertension, diabetes, stroke or seizures. He reported a family history of hearing loss in his father, who also worked around farm equipment, and denied a family history of hearing loss otherwise.
O: Otoscopic examination showed clear ear canals with no abnormalities of either pinna; tympanic membranes were pearly grey with no bulging or retraction; the malleus and umbo were clearly visible at both ears. Pure tone air and bone conduction testing indicated bilateral mild-moderate sloping sensorineural hearing loss. Speech recognition thresholds were in agreement with pure tone testing. Word recognition ability in quiet appeared excellent (96% at the right ear and 94% at the left ear). Tympanometry measures were WNL at both ears. Ipsilateral and contralateral acoustic stapedial reflexes were present at 500 and 1000 Hz at both ears and were absent at 2000 and 4000 Hz.
A: Bilateral mild-moderate sensorineural hearing loss. The hearing loss is consistent with the patient’s history of noise exposure. Hearing is impaired to the extent that that the patient is likely to have difficulty communicating, particularly in noisy situations, in stressful situations, and/or when he is feeling tired or unwell. Mr. Walker is a likely candidate for amplification and aural rehabilitation.
P: An amplification evaluation was scheduled and the patient was provided with some general information about hearing aids to review in the meantime. Use of a personal amplifier such as a pocket talker as a short-term solution to difficulty hearing his health care providers is recommended and was discussed. The patient was advised to keep a written record of instructions given to him by his health care providers, particularly given his concern about missing important information.
Electronically signed by Teri Westlake, AuD
Dental Clinical Note
Dental Clinical Notes
Patient Name: Bobby Walker
Date of Birth: 07/04/1984 (Age 41)
Date of Visit: [ 1.5-2 weeks post-ER visit]
Referring Provider: ER Physician/PCP following fall
S: Subjective
Mr. Bobby Walker presents for urgent dental evaluation following a fall approximately 1.5 weeks ago, which resulted in a fractured wrist and injuries to his mouth, teeth, and lips. He reports significant pain and difficulty speaking due to the lip injury and fractured teeth. He expresses concern about the financial impact of his current health issues, including the newly diagnosed COPD, and the time commitment for various medical appointments.
Chief Complaint: "Busted teeth and it's hard to talk because the teeth that fractured when I fell pushed through my lip."
History of Present Illness (HPI): Patient states that during a recent training run for a "Couch to 5K" event, he experienced severe shortness of breath, causing him to stumble and fall. Upon impact, his head struck the ground, leading to a left wrist fracture (dominant hand) and oral trauma. He reports fractured teeth, a lip injury where teeth "pushed through," and gum injuries. He states the lip injury makes it "hard to talk."
Medical History (Relevant):
- Asthma (long-standing)
- Newly diagnosed Chronic Obstructive Pulmonary Disease (COPD)
- History of 3 packs/day cigarette smoking for many years, quit ~1 year ago.
- Current chewing tobacco use (started ~1 year ago).
- Recent left wrist fracture (underwent closed reduction in ER, currently in a half-cast, fingers stiff and swollen, difficulty with ADLs).
- Complaint of difficulty hearing providers in ER; wife notes history of frequently asking her to repeat.
- Complaints of knee, lower back, and foot pain.
- Reports significant stress and grief due to the death of his son, Noah, in April 2024.
- Financial concerns related to his wife's being on unpaid medical leave (due to vocal fold issues) and his own potential missed work for appointments.
- Resides in a third-floor apartment, which is becoming difficult to navigate due to breathing issues.
Dental History:
The patient reports prior tooth decay and expresses concern about "gray patches in my mouth," as noted by the ER dentist. No recent dental visits were mentioned before the fall.
O: Objective
Vital Signs:
Within normal limits for a patient with controlled COPD, but the patient presents with observable shortness of breath during conversation, requiring frequent pauses to breathe. Oxygen saturation is stable (based on ER notes).
Extraoral Examination:
- Face: Appears pale and fatigued.
- Lips: Significant swelling and lacerations noted on the lower lip, consistent with tooth avulsion/penetration. Erythema and possible bruising around the perioral area. Patient reports pain on palpation.
- TMJ: No apparent deviation or limited opening.
- Lymph Nodes: No palpable lymphadenopathy.
Intraoral Examination:
- Oral Mucosa:
- Buccal Mucosa: "Gray patches" noted bilaterally on buccal mucosa, suggestive of nicotine stomatitis or smokeless tobacco keratosis. The area appears slightly thickened and corrugated. Further observation is needed.
- Floor of Mouth/Tongue: Appears unremarkable.
- Gingiva: Generalized inflammation and erythema, particularly in areas adjacent to fractured teeth. Lacerations are present on the mandibular anterior gingiva.
- Dentition:
- Maxillary Anterior: Fractured incisal edges on #8 and #9 (likely enamel and dentin involvement, possible pulp exposure). Percussion sensitivity positive on #8, #9. Mobility checked: negative.
- Mandibular Anterior: Fracture of crown #24 (possible subgingival fracture, pulp exposure likely). Tooth #25 exhibits significant mobility (Grade II) and displacement, indicating probable luxation or avulsion. Bleeding noted from the gingival sulcus around #24 and #25.
- Posterior Dentition: Multiple existing restorations observed. Initial visual assessment reveals active carious lesions on #3 (occlusal), #14 (mesial-occlusal), and #19 (occlusal-buccal).
- Occlusion: Appears stable on posterior teeth; however, anterior trauma disrupts regular occlusal contacts.
Radiographic Findings (Assumed, based on typical ER/dentist workup):
- Periapical radiographs of #8, #9, #24, #25 reveal:
- #8, #9: Fractured crown, no obvious root fracture or periapical pathology.
- #24: Crown fracture extending to the root with periapical radiolucency, suggesting pulpal necrosis.
- #25: Evidence of root fracture or avulsion.
- Bitewing radiographs: Confirm carious lesions on #3, #14, #19.
- Panoramic radiograph: No gross pathology noted in the jaws or TMJ. Evidence of generalized alveolar bone loss consistent with periodontal disease in some areas.
A: Assessment (Dental Diagnoses)
- Traumatic Dental Injuries:
- Fractured Teeth: #8, #9 (complicated crown fractures), #24 (complicated crown-root fracture).
- Luxated/Avulsed Tooth: #25 (possible complete avulsion or severe lateral luxation).
- Soft Tissue Trauma: Lacerations of lower lip, gingival lacerations (mandibular anterior).
- Dental Caries:
- Active carious lesions: #3 (occlusal), #14 (mesial-occlusal), #19 (occlusal-buccal).
- Oral Mucosal Lesions:
- Suspected Nicotine Stomatitis/Smokeless Tobacco Keratosis: Bilateral buccal mucosa.
- Periodontal Disease:
- Generalized gingivitis (due to inflammation, possibly a contributing factor from tobacco).
- Evidence of generalized chronic periodontitis based on radiographic bone loss.
- Risk Factors:
- Current chewing tobacco use (high risk for oral cancer, periodontal disease).
- Former heavy cigarette smoker (increased risk for periodontal disease, oral cancer, impaired healing).
- Poor oral hygiene (implied by existing decay and gingivitis).
- Stress and grief (potential impact on self-care and immune response).
- COPD (potential impact on overall health, tolerance for procedures, increased risk of infection).
P: Plan (Treatment Plan)
The primary goals of treatment are to address acute trauma, alleviate pain, restore function and aesthetics, manage existing dental disease, and provide comprehensive oral health education, particularly regarding tobacco use. This plan will need to be coordinated with his overall medical care due to his COPD, wrist fracture, and other systemic issues.
Prognosis: Fair to good, highly dependent on patient compliance with tobacco cessation and commitment to the extensive treatment plan. His medical comorbidities (COPD, wrist injury) and psychosocial factors (grief, financial strain) will be significant considerations impacting adherence and outcomes.
Occupational Therapy Initial Evaluation Note
Patient Name: Bobby Walker
Date of Birth: 07/04/1984
Visit No: 1- Initial evaluation
Setting: Outpatient hand therapy
Diagnosis: Left comminuted and angulated distal radial fracture (colles); closed reduction successful; Left ulnar styloid fracture: stable.
M.D. Orders: OT eval. and treatment. Fabricate orthoplastic, removable ventral wrist cock-up orthosis; begin P/AROM of hand and elbow with splint in place.
Precautions: Non-weight bearing (NWB) on left wrist.
SUBJECTIVE
History of Present Condition/Mechanism of Injury:
Patient fell onto his outstretched left arm 2 weeks ago during a 5K run. He was seen in the emergency
room of the local hospital for follow-up later that same day. X-rays showed a Left wrist distal radial
and ulnar fracture. Closed reduction of the displaced fracture was successful as evidenced with
post-reduction films. A left orthoglass splint was applied in the ER prior to discharge: long arm
sugar-tong with thumb spica applied. Patient had follow-up with the orthopedic specialist and presents
with new script of OT eval. and custom orthotic fabrication.
The patient also received a Home Health OT evaluation for a one-time home safety and functional
assessment. Patient and caregiver were provided with resources, adaptive strategies, and safety
checklist.
PMH: Chronic Obstructive Pulmonary Disease. Shortness of breath. Decreased hearing acuity. Chronic pain (knee, foot, low back)
Primary Concern/Chief Complaint:
Patient reports difficulty with ADLs due to fatigue, pain, and inability to use dominant left hand
functionally secondary to the L distal radius fracture. He is currently off duty as a railroad engineer
and is concerned about a lengthy time without working.
Handedness: Patient is Left hand dominant
Current Level of Function (PLOF):
Self-Care/ADLs: Home Health OT Barthel Index score: 80/100. He reports difficulty with buttons/zippers while dressing. Unable to open bottles and containers during ADL tasks.
Mobility: Needs rest breaks and railing when climbing stairs.
IADL: Low endurance secondary to COPD affects IADL functioning. He is currently not driving. Plans to be off work for 6 weeks and then will return on light duty for 4 weeks.
Leisure/Interest: Patient wants to continue with increasing physical activity and would like to try for another 5K run later this year. He likes to read the newspaper and watch movies.
Employment history: FT Railroad engineer. He must have full strength and motion in his left hand for return to normal duty.
Home Layout: See Home Health OT eval.
Pain Location:
Worst: 6/10; Best: 2/10; Current: 4/10
Description of Pain: Aching pain in left wrist and hand at rest. He reports sharp pain in the ventral wrist with gripping of the left fingers and opposition of the left thumb. He reports ‘stiffness’ throughout the left hand.
Mental Status/Cognitive Function: Intact
Patient Goals: Regain ability to use left hand and wrist functionally for return to driving and for all work tasks.
OBJECTIVE
Patient Consent
Patient/Consent: X
Objective Measures
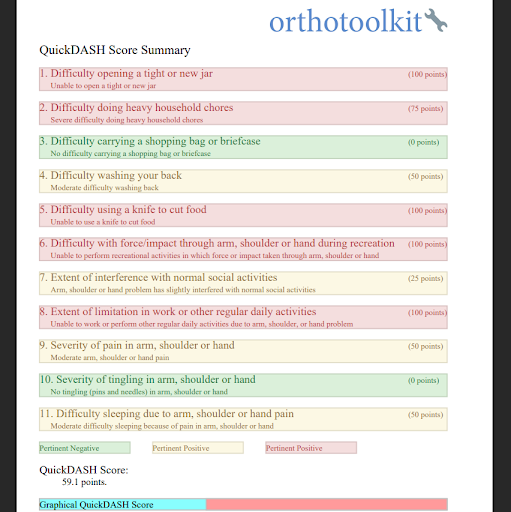
Quick Dash: 59.1% perceived disability. See attached report.
Cast/Splint Type: Orthoplastic ventral wrist cock-up splint fabricated this date. Good fit achieved; patient instructed in wear and care of orthosis including skin inspection and wearing schedule. He is to wear splint at all times for the next 2 weeks except during hand hygiene and showering. He was independent with don/doff of splint.
Range of Motion
| Elbow AROM | Right | Left |
| Extension | WNL | WNL |
| Flexion | WNL | WNL |
| Supination | WNL | 45 degrees |
| Pronation | WNL | 55 degrees |
| Wrist AROM | Right | Left |
| Extension | WNL | NT |
| Flexion | WNL | NT |
| Radial Deviation | WNL | NT |
| Ulnar Deviation | WNL | NT |
| Hand AROM | Right | Left |
| Thumb MP | ||
| Extension/Flexion | WNL | 0/20 degrees |
| Thumb IP | ||
| Extension/Flexion | WNL | 20/60 degrees |
| Finger pulp-DPC | ||
| IF | WNL | 6 cm |
| MF | WNL | 7 cm |
| RF | WNL | 8 cm |
| SF | WNL | 10 cm |
| Comments: | Patient reports severe stiffness when attempting to make a fist. |
Hand Strength: Not tested due to healing left distal radius fracture.
Coordination
| Reciprocal opposition | Right | Left |
| WNL | Able to bring thumb to tip of IF, MF, and RF. Unable to touch tip of SF. |
Edema:
Wrist circumference:
Right: 19 cm Left: 23 cm
ASSESSMENT:
Assessment/Diagnosis:
The patient presents with signs and symptoms consistent with a diagnosis of distal radius fracture, 2 weeks post injury. The newly fabricated orthosis fits well and will allow for the patient to have unobstructed movement of the fingers and thumb for AROM and light hand use for ADLs. Edema and stiffness in the left hand decreases his ability to grip and pinch which hinders his ability to complete ADL tasks. He displays limited forearm rotation which affects left hand use for self-feeding, peri-care, and oral hygiene.
Recommend skilled OT for hand therapy to work toward goals. We will begin with wrist motion and strengthening of the hand and wrist as per M.D. order as bone healing progresses.
Rehab Potential: Good
Problem list:
Pain with functional use of Left hand
Decreased AROM of fingers and thumb on the left
Edema in left
wrist
Decreased forearm rotation on the left
Decreased grip and pinch strength
Long Term Goals (8 Weeks):
- Patient will exhibit WNL AROM of left hand and thumb for cutting food with a knife.
- Patient will have >60# strength for opening tight jars.
- Patient will report '<'2 /10 pain with work simulated activities as a railroad engineer.
- Patient will tolerate work simulated lift and carry 20# for 30 min. before fatigue.
Short Term Goals:
- Patient will be independent with wear and care of orthosis including skin inspection.
- Patient will exhibit WNL 3-pt. pinch for writing x 5 minutes with left hand.
- Patient will have WNL grip for use left hand for oral hygiene.
- Patient will exhibit >65 degrees wrist flexion and extension for getting dressed independently.
- Patient will exhibit WNL forearm rotation for keyboard work.
PLAN
Frequency: 3x/week
Duration: 8 weeks
Plan: Preparatory methods- modalities as indicated, soft tissue massage, P/AAROM, therapeutic exercises. Therapeutic activities- functional activities to work on hand strength, wrist stability, weight-bearing, and normal motion. Occupational activities- ADLs/IADLs, work simulated activities.
Signature: Tania Shearon, OTR/L, CHT Date: 00/00/2025
Occupational Therapy Home Evaluation Note
Patient: Bobby Walker | Age: 41
Occupational Therapy Home Evaluation
Diagnosis:
Left wrist fracture, COPD, Asthma, Chronic Pain (knee, foot, low back)
Referral Reason:
Home safety and functional evaluation is requested following recent fall, new COPD diagnosis, and reported decline in ADLs.
Background Summary:
Mr. Bobby Walker is a 41-year-old male residing in a third-floor walk-up apartment with his wife,
Brianne, in Decatur, Illinois. He is currently recovering from a left wrist fracture sustained in a fall
while training for a memorial 5K in honor of his late son, Noah, who passed away in a military training
accident. Mr. Walker has a history of chronic respiratory conditions, including asthma and a recent
diagnosis of COPD, which, along with musculoskeletal pain in his back, knees, and feet, significantly
limit his mobility, endurance, and safety during daily activities.
Following his fall, Mr. Walker also sustained oral trauma, resulting in fractured teeth, gum and lip
injuries, and is currently under dental evaluation for both acute injury and concerning findings,
including gray patches and tooth decay. He also experiences hearing difficulties, likely due to
long-term noise exposure at work and recreational events such as truck and tractor pulls, which affect
his ability to follow conversations and medical instructions, especially in noisy environments like the
ER.
Mr. Walker reports increasing difficulty with self-care tasks, including dressing, grooming, and safely
navigating his apartment environment due to his respiratory status, wrist injury, and overall physical
limitations. His wife, Brianne, who has vocal fold dysfunction causing hoarseness and vocal fatigue,
serves as his primary support person. However, her communication difficulties and her current medical
leave due to her condition have created additional emotional and financial stress. The couple is
grieving the loss of their son, managing chronic health conditions, and coping with multiple
environmental, physical, emotional, and financial barriers that impact their overall quality of life and
ability to access care.
Evaluation Tool:
Barthel Index of Activities of Daily Living: (See attachment)
Home Environment:
- Home Layout: Third floor, no elevator—significant fall and respiratory risk.
- Bathroom: No grab bars, step-in tub, limited ventilation.
- Bedroom: Bed is low; minimal space for walker/crutches if needed.
- Kitchen: High cabinets limit access with dominant hand in cast.
- Entryway: Cluttered and lacks sturdy handholds.
OT Assessment:
Mr. Walker presents with moderate limitations in daily living activities due to fatigue, pain, and limited left-hand use. COPD symptoms and emotional strain further decrease safety and independence. Environmental barriers (stairs, clutter, bathroom setup) elevate fall risk and may limit recovery. Brianne (wife) shows signs of caregiver strain, complicated by her own vocal limitations.
Interventions:
- Caregiver Education: Instructed Brianne in safe transfer techniques, energy conservation, and how to assist without straining herself. Provided written strategies for fall prevention and safe meal setup.
- ADL Strategies: Taught adaptive techniques for grooming, dressing with one hand, and meal prep with low energy.
- Equipment Recommendations:
- Non-slip bath mat
- Tub transfer bench
- Grab bars (bathroom and near bed)
- Long-handled reacher and shoehorn
- Environmental Modification Suggestions:
- Remove tripping hazards (e.g., entry clutter)
- Organize commonly used items within reach
- Consider relocation to lower floor or elevator-accessible unit if possible
Short-Term Goals (to be carried out independently):
- Mr. Walker will complete basic ADLs (dressing, grooming, toileting) with use of adaptive techniques and rest breaks as needed.
- Mr. Walker and caregiver will apply energy conservation daily to complete ADLs.
- Brianne will demonstrate understanding of safe assist strategies and use caregiver support tools as needed.
- Bobby will attend OT evaluation hand therapy for continued care.
Plan:
No further OT home visits required at this time.
Bobby demonstrates functional independence in activities of daily living (ADLs) with minor adaptations. He presents as oriented, cognitively intact, and highly motivated to improve. With consistent caregiver support from his spouse, Brianne, and his own personal drive, continued progress is anticipated. At this time, ongoing home health occupational therapy visits are not indicated. However, a referral to OT evaluation for hand therapy is recommended to address specific upper extremity needs and support his continued recovery.
SOAP Note:
S (Subjective):
Pt states: "I can’t catch my breath walking up these stairs. I want to do more, but everything is harder now with my wrist and lungs."
O (Objective):
- Moderate dyspnea with stair climbing; required seated rest upon entry.
- Left UE in cast; unable to perform fine motor tasks independently.
- Barthel Index: 80/100 – Mild Dependence in ADLs.
- Bathroom and kitchen environments pose safety concerns.
A (Assessment):
Pt demonstrates moderate dependence in ADLs due to musculoskeletal and respiratory issues. Home environment poses significant barriers to safety. Caregiver capable but in need of education and support. Emotional and physical stress are contributing to decreased functional performance.
P (Plan):
This was a one-time home safety and functional assessment.
- No further in-home OT visits scheduled at this time but recommendation for OT evaluation for hand therapy. Follow up with dentistry and audiology. Recommendation for social work or mental health therapy to address grief, coping, and family support.
- Pt and caregiver provided with written resources, adaptive strategies, and safety checklist.
- Encouraged to contact OT services for reassessment if condition worsens, home situation changes, or new safety concerns arise.
Barthel Index of Activities of Daily Living – Bobby Walker
| Activity | Score | Justification |
| Feeding | 10 | Independent. Can use nondominant hand with adapted technique; no feeding issues. |
| Bathing | 5 | Requires supervision or minimal assistance due to fatigue and slippery surfaces. |
| Grooming | 5 | Independent with setup; uses nondominant hand for basic grooming tasks. |
| Dressing | 5 | Manages with effort; needs help with buttons/zippers due to wrist but compensates. |
| Bowels | 10 | Continent. No issues reported. |
| Bladder | 10 | Continent. No issues reported. |
| Toilet Use | 10 | Independent. Able to manage hygiene and transfers with adaptive technique. |
| Transfers (Bed to Chair) | 10 | Independent. May use armrests or furniture for support but stable. |
| Mobility (on level surfaces) | 10 | Walks independently short distances; mild shortness of breath with exertion. |
| Stairs | 5 | Able to ascend/descend stairs slowly with railing and rest breaks. |
Total Score: 80/100
Interpretation: Mild Dependence
Occupational Therapist: Melissa Yeung OTD, OTR/L
Physical Therapy Note
PHYSICAL THERAPY NOTE
Patient Name: Bobby Walker
Age: 41 years old
DOB: 07/04/1984
Marital Status: Married
Spouse: Brianne
Son: Noah (deceased, killed in a military training accident in 2024)
Daughter-in-Law: Ella
Grandson: Ty
Ethnicity: Caucasian
Date of Referral: X/XX/2025
Date of PT evaluation: X/XX/2025
S:
C/C:“I really want to use my left hand now, but it’s just so painful to move it!”
History:
This patient was referred to this clinic by the orthopedic surgeon for further PT evaluation and treatment. The patient sustained a left wrist fracture after he stumbled and fell during one of his practice runs. He underwent a closed reduction procedure and was placed in a half cast. He currently rates his pain at 8/10 when moving the fingers and 5/10 at rest. The patient stated that he was preparing for a 5K marathon as he wanted to get back into shape. While he quit smoking a year ago, he reported having more issues with his breathing. Recently, he was diagnosed with COPD on top of his prior asthma diagnosis. Patient stated that he has been a heavy smoker since he was a teenager. He also reported pain in his right knee, lower back, and right foot. He also admitted that he is beginning to lose his hearing. With everything that has been happening to his body, the patient stated that he is very concerned that these will impact his income and concerned that he won’t be able to fully support his wife and pay all the bills. He is also concerned that his activities at home have been severely limited due to his wrist injury. The patient is left hand dominant.
Social history:
- Lives with wife Brianne who is currently on medical leave from her job teaching high school chorus due to diagnosis and treatment for having vocal fold issues
- Son Noah died in 2024 during his army training, leaving behind his wife and son Ty who both live two hours away in St. Louis
- Daughter-in-law is a practicing nurse
- Patient and wife live in a very supportive neighborhood, but admitted that all their friends are also busy with work and family life
O:
V/S: BP – 130/80 mmHg
HR – 65 bpm
RR – 18 cpm
PR – 85 bpm
Ocular inspection:
- Patient was alert and coherent
- Cast in place (left wrist); no visible discoloration of left finger nail beds
- Left hand appears swollen
Manual Muscle Testing:
- All group muscles grossly graded 5/5, except for left upper extremity – not tested as patient did not consent due to fear and pain
Myotome Testing:
- Grossly graded 5/5 on all 4s, except for left C5-T1 – not tested as patient did not consent
Sensory Testing:
- Grossly graded 2/2 (light touch and pin prick for pain), except for left C6-T1, not fully tested at this time
Range of motion
- Full ROM on all 4s except for:
- left elbow, wrist, and hand – not tested at this time
- right knee: 0-83 degrees, limited by pain at end range [left knee: 0-110]
- right foot PF: 0-15 [left foot PF: 0-36]
- left foot DF: 0-17 [left foot DF: 0-25]
Muscle palpation – tenderness noted above cast and left fingers
A:
PT Impression: Patient presents with limited left hand mobility secondary to pain and cast restrictions.
His dermatome and myotome are grossly WNL, except for the areas noted above, particularly left upper
extremity. Functional limitations include limited activities at home as he is left hand dominant. While
he lives with a supportive wife, patient expressed concern about their financial situation due to his
recent wrist injury. It is anticipated that the patient will have good prognosis. At this point, the
focus of PT will be on the left wrist while at the same time providing patient with advice on energy
conservation techniques as he reported that his shortness of breath has become severe. Other issues
related to his back, knee, and foot will be addressed later once the patient’s current chief complaint
has been addressed adequately. These other affected areas will have an impact on the patient’s plan to
eventually go back to practicing runs again in preparation to joining a 5K marathon.
Problem lists:
- Limited ROM of left wrist/hand due to swelling and pain
- Limited ROM right knee with pain at end range
- Limited ROM left foot
- Reported low back pain
P:
Short term:
- Educate patient on techniques to prevent worsening of left hand swelling
- Educate on energy conservation techniques
- AROM exercises on left fingers
- Patient education re: monitoring of circulation on right hand (i.e. nail bed coloration)
- Refer patient to OT for further evaluation and assessment
Medium term:
- Address anticipated decreased range of motion in left hand and wrist
- Address anticipated decreased strength in left hand and wrist muscles
- Continue working on building patient’s endurance level
Signed: John Doe, PT
XX/XX/2025
Public Health Note
Health Science/Public Health Education:
Patient Educator and Navigator
Case Notes
Certified Health Education Specialists (CHES) have versatility and skillsets to practice in many different career settings, across the country and even overseas. Job titles in the hospital and healthcare sector can vary. Some common titles include Community Benefits Manager, Outreach Manager, Patient Educator or Program Manager, Patient Navigator, Wellness Coordinator, and Health Educator. Health Education Specialists in the Health Care setting may perform the following duties:
Deliver and assess health education programs; Coordination and outreach
Enrollment and initial health assessments; Motivate others to initiate behavior change
Communicate/liaise with primary care physicians, hospitals and other health care providers
Plan for health education interventions; Translate medical and health education material for dissemination to client/patient
- Recommendations for patient/family Education and Resources from the CHES Patient Educator
Patient [Bobby Walker] Education and Resources
- Tobacco education/cessation:
FOR PROVIDERS – clinical education/guidance and resources
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000001293
https://www.cancer.gov/about-cancer/causes-prevention/risk/tobacco/smokeless-fact-sheet
https://www.cdc.gov/tobacco/other-tobacco-products/smokeless-product-use-in-the-us.html
https://www.cdc.gov/tobacco/other-tobacco-products/smokeless-tobacco-health-effects.html
https://www.cancer.org/cancer/risk-prevention/tobacco/smokeless-tobacco.html
https://www.cdc.gov/tobacco/hcp/patient-care/clinical-cessation-tools.html
https://www.cdc.gov/tobacco/hcp/patient-care/patient-cessation-materials.html
https://www.cdc.gov/tobacco/hcp/patient-care/clinical-education-and-training.html
FOR PATIENT/FAMILY
https://quityes.org/free-services/
https://www.cancer.org/cancer/risk-prevention/tobacco/guide-quitting-smoking.html
https://www.lung.org/quit-smoking
https://www.cdc.gov/tobacco/about/how-to-quit.html
https://smokefree.gov/quitting-dip
https://www.cdc.gov/tobacco/hcp/patient-care/quitlines-and-other-resources.html
https://www.lung.org/quit-smoking/help-someone-quit
Local resources:
https://www.maconchd.org/healthy-living
- Asthma education:
FOR PROVIDERS – clinical education/guidance and resources
https://www.lung.org/lung-health-diseases/lung-disease-lookup/asthma/resource-library
https://www.cdc.gov/asthma/hcp/clinical-guidance/index.html
https://www.lung.org/lung-health-diseases/lung-disease-lookup/asthma/health-professionals-educators
https://www.nhlbi.nih.gov/node-general/asthma-resources-health-professionals
https://education.aaaai.org/asthma-education
FOR PATIENT/FAMILY
https://www.lung.org/help-support/lung-helpline/navigators
https://www.lung.org/lung-health-diseases/lung-disease-lookup/asthma
https://www.cdc.gov/asthma/living-with/index.html
https://healtheducationstore.lung.org/
https://aafa.org/asthma/living-with-asthma/asthma-in-adults/
https://aafa.org/asthma/asthma-triggers-causes/exercise-induced-asthma/
https://www.asthmacommunitynetwork.org/programs/illinois-asthma-program-0
- COPD/COPD and Exercise:
FOR PROVIDERS – clinical education/guidance and resources
https://www.lung.org/lung-health-diseases/lung-disease-lookup/copd/for-health-professionals
https://goldcopd.org/2024-gold-report/
https://www.nhlbi.nih.gov/health/copd
https://www.thoracic.org/statements/resources/copd/179full.pdf
https://bestpractice.bmj.com/topics/en-us/7/guidelines
https://www.ncbi.nlm.nih.gov/books/NBK559281/
PULMONARY REHAB
https://www.nhlbi.nih.gov/health/pulmonary-rehabilitation
https://pmc.ncbi.nlm.nih.gov/articles/PMC7515680/
https://memorial.health/medical-services/lung-care/
https://www.dcmh.net/health-services/rehabilitation/pulmonary-rehabilitation/
https://memorial.health/memorial-specialty-care-pulmonology/overview/
https://www.hshs.org/st-marys-decatur/services/pulmonary
FOR PATIENT/FAMILY
https://www.nhlbi.nih.gov/health/copd/living-with
https://www.lung.org/lung-health-diseases/lung-disease-lookup/copd
https://www.lung.org/lung-health-diseases/wellness
https://www.cdc.gov/copd/index.html
https://www.nhlbi.nih.gov/resources/quick-guide-copd
https://www.nhlbi.nih.gov/health-topics/education-and-awareness/copd-learn-more-breathe-better
https://www.cdc.gov/cdi/indicator-definitions/chronic-obstructive-pulmonary-disease.html
https://www.nhlbi.nih.gov/sites/default/files/publications/take_action_on_copd_fact_sheet.pdf
https://www.lung.org/lung-health-diseases/wellness/breathing-exercises
AND EXERCISE.
https://www.lung.org/lung-health-diseases/wellness/exercise-and-lung-health
https://pmc.ncbi.nlm.nih.gov/articles/PMC9354440/
https://pmc.ncbi.nlm.nih.gov/articles/PMC11167654/
https://health.clevelandclinic.org/have-copd-exercise-helps-keep-you-out-of-the-hospital
https://pmc.ncbi.nlm.nih.gov/articles/PMC12009044/
https://www.thoracic.org/patients/patient-resources/resources/exercise-with-lung-disease.pdf
- Family counseling/mental health:
FOR PATIENT/FAMILY
https://www.crossinghealthcare.org/behavioral-health
https://www.freementalhealth.us/county/il-macon
https://www.mentalhealthcenters.net/clinics/illinois/macon-county.html
- Other resources:
NS Railroad – health benefits/insurance carrier/coverage:
http://bletns.com/html/benefit_information.html
http://www.bletns.com/html/blet_ns_short_term_disability.html
Financial assistance/medical bills
https://www.needhelppayingbills.com/html/macon_county_assistance_progra1.html
https://www.needhelppayingbills.com/html/macon_and_sangamon_catholic_ch.html
https://www.doveinc.org/programs/max-dax
Respite care
https://search.ne211.org/search/b91e1fee-0f8e-5cbc-abc5-03bb0a08f70c
https://synergyhomecare.com/il-decatur-62521/respite-care-resources/
https://www.dhs.state.il.us/page.aspx?item=163600
Low cost health centers
https://www.healthcenterclinics.org/center/community-health-improvement-center/
Speech-Language Pathology Note
Speech-Language Pathology assessment
Client Name: Walker, Bobby
DOB: 07/04/1984
Subjective:
Pt. is a 41-year-old male referred by his primary care physician in order to assess swallowing and speech concerns after the patient sustained a fall which resulted in some facial and dental injuries as well as a fractured wrist. The patient was accompanied by his wife. Pt. indicated “I have experienced more pain when swallowing” since his injury. He indicated he “sometimes” coughs during meals. He also noted that his speech has been less clear since his fall. Pt. is concerned about communicating clearly when he goes back to work as a railroad engineer. Pt.’s history also includes a diagnosis of COPD. He reported a 3 pack/day smoking habit up until one year ago, and he reported current use of chewing tobacco. The patient’s wife also noted that she is concerned about his hearing since he frequently asks her to repeat herself.
Objective:
An oral peripheral exam revealed the following:
- Swelling of the lower lip with mildly reduced range of motion.
- Dental fractures to maxillary and mandibular central incisors. Right mandibular central incisor appears loose and twisted. Pt. reported occasional bleeding from the gums at this location.
- Gray-ish discoloration of the buccal mucosa. (Notes from dental evaluation reported possible nicotine stomatitis or smokeless tobacco keratosis in the buccal mucosa, for which he will follow up with his dentist or other professionals, as needed.)
- All other structures (e.g., hard palate, soft palate, tongue, fauces) and their associated functions were within functional limits.
An informal observation of conversational speech revealed minor distortions of vowels /u/, /o/, and /ʊ/ as well as distortions on consonants /w/, /b/, /p/, /m/, /f/, and /v/. In a known context, the patient’s speech was 100% intelligible.
In decontextualized situations (e.g., randomized sentences from the Assessment of Intelligibility of Dysarthric Speech) with the patient facing away from the clinician, the pt. was 85% intelligible.
A clinical evaluation of swallowing was conducted to determine any strategies for increased pt. comfort during eating as well as to screen for safety when eating and drinking. The following consistencies were administered in varying amounts: thin liquids, nectar-thick liquids (mildly thick), pureed, mechanical soft (minced and moist), and regular. Patient preferred to drink by straw; however, several trials were completed without a straw (cup sips).
Liquids:
Pt. indicated a pain rating of 4/10 when sipping mildly thick liquids through a straw. Pain reduced to 2/10 with thin liquids through a straw. For all liquid presentations by straw, pt. exhibited mildly reduced lip seal with occasional anterior spillage of liquids (mostly with thin liquid presentations). Laryngeal elevation during all swallows was timely with good ROM. Pt. was noted to clear his throat 3/10 trials during or shortly after laryngeal elevation with thin liquids by straw. Vocal quality returned to baseline after all swallows. During 5 trials of thin liquids without the straw (i.e., cup sips), no throat clearing events were noted, and voice quality remained at baseline.
Foods:
Pt. indicated no significant pain level with pureed or mechanical soft consistencies; however, he indicated a pain level of 3/10 for regular solids. The patient further clarified that he felt fatigued when chewing for a prolonged period of time. For all food consistencies, the patient demonstrated adequate oral preparation of foods with good oral clearance of all bolus types. Laryngeal elevation was timely with good ROM and strength. No overt signs/symptoms of possible aspiration were noted with food consistencies.
Pt. was provided with education on speech intelligibility strategies as well as strategies for increased safety and comfort with swallowing while healing from his injuries. Pt. was encouraged to seek an audiological evaluation to follow up on family concerns about his hearing.
Assessment:
Pt. presents with mild speech intelligibility disruptions due to physical trauma involving the lips and teeth. Pt. displayed mild oral dysphagia due to physical trauma, characterized by occasional anterior spillage of thin liquids when drinking by straw. Pt. displayed possible signs/symptoms of aspiration (i.e., throat clearing) on 3/10 thin liquid swallows by straw. No overt signs/symptoms of aspiration were noted when taking smaller sips by cup.
Plan:
Recommend:
- Pt. should utilize speech intelligibility strategies while healing from his injuries. Strategies were taught in today’s session and provided via handout.
- Recommend pt. consume a mechanical soft diet with thin liquids for 2-4 weeks while healing from injuries. Pt. should re-assess his pain level with regular solids after that point.
- Recommend small sips of thin liquids by cup (no straw). If patient notes increased coughing with meal/liquid intake, he should seek a referral for a modified barium swallow study to better assess the safety of his pharyngeal swallow.
Workshop Recordings
Workshop 1: Whole Person Healthcare
Workshop 2: Roles and Responsibilities
Workshop 3: Social and Medical Impacts of Untreated Hearing Loss in Adults
Learn more about the roles and responsibilities of the care providers
Athletic trainers
Athletic Trainers use a medical based model to provide comprehensive patient care in the domains of prevention; clinical evaluation and diagnosis; immediate and emergency care; treatment and rehabilitation; and organization and professional health and well-being. Athletic Trainers are highly qualified, multi-skilled health care professionals who collaborate with physicians to provide total patient care. Athletic Trainers work under the direction of a physician as prescribed by state licensure statutes.
Learn more at: http://www.nata.org/
Audiologist
"An audiologist is a person who, by virtue of academic degree, clinical training, and license to practice, is uniquely qualified to provide a comprehensive array of professional services related to the identification, diagnosis and treatment of persons with auditory and balance disorders, and the prevention of these impairments. Audiologists serve in a number of roles including primary service provider, clinician, therapist, teacher, consultant, researcher and administrator. In addition, the supervising audiologist maintains legal and ethical responsibility for all assigned audiology activities provided by audiology assistants and audiology students."
Source: Academy of Doctors of Audiology
Counselor
What is professional counseling?
“Professional counselors help people gain personal insights, develop strategies and come up with real-life solutions to the problems and challenges they face in every area of life. As trained and credentialed professionals, they accomplish this by getting to know clients, by building safe, positive relationships and suggesting tools and techniques they believe will benefit clients.”
Learn more at: https://www.counseling.org/mental-health-counseling/what-is-counseling
Dentist
What is a Dentist?
You will find an interesting article here about the important interconnection between oral health and systemic health. So don't forget the importance of collaborating with the dentist!
Doctor of osteopathic medicine
“Doctors of Osteopathic Medicine use a unique whole-person approach to help prevent illness and injury.
Accounting for approximately 11% of all physicians in the United States, Doctors of Osteopathic Medicine, or DOs, bring a unique, patient-centered approach to every specialty across the full spectrum of medicine. They are trained to listen and partner with their patients to help them get healthy and stay well.”
Learn more at: https://osteopathic.org/what-is-osteopathic-medicine/what-is-a-do/
Nursing:
Registered Nurses
“Registered nurses (RN) form the backbone of health care provision in the United States. RNs provide critical health care to the public wherever it is needed.
Key Responsibilities
- Perform physical exams and health histories before making critical decisions
- Provide health promotion, counseling and education
- Administer medications and other personalized interventions
- Coordinate care, in collaboration with a wide array of health care professionals”
Occupational therapist
Occupational therapy is the only profession that helps people across the lifespan to do the things they want and need to do through the therapeutic use of daily activities (occupations). Occupational therapy practitioners enable people of all ages to live life to its fullest by helping them promote health, and prevent—or live better with—injury, illness, or disability.
Common occupational therapy interventions include helping children with disabilities to participate fully in school and social situations, helping people recovering from injury to regain skills, and providing supports for older adults experiencing physical and cognitive changes.
Occupational therapy practitioners have a holistic perspective, in which the focus is on adapting the environment and/or task to fit the person, and the person is an integral part of the therapy team. It is an evidence-based practice deeply rooted in science.
See also: https://www.aota.org/career/become-an-ot-ota/about-the-profession
Learn more at: AOTA.org
Physical therapist
Physical therapists are movement experts who optimize quality of life through prescribed exercise, hands-on care, and patient education. After making a diagnosis, physical therapists create personalized treatment plans that help their patients improve mobility, manage pain and other chronic conditions, recover from injury, and prevent future injury and chronic disease.
Physical therapists empower people to be active participants in their own treatment, and they work collaboratively with other health professionals to ensure patients receive comprehensive care. Physical Therapy entry-level educational programs are at the doctoral level with subsequent educational opportunities for fellowship and residency. Physical therapists work in a wide range of specialty areas for which they can obtain specialty certification e.g. acute care, aquatics, cardiovascular & pulmonary, geriatrics, home health, neurology, oncology, orthopedics, pediatrics, sports, and women's health.
See Also: https://www.apta.org/your-career/careers-in-physical-therapy/becoming-a-pt
Learn more at: apta.org
Physician assistant
What is a PA?
“PAs (physician associates/physician assistants) are licensed clinicians who practice medicine in every specialty and setting. Trusted, rigorously educated and trained healthcare professionals, PAs are dedicated to expanding access to care and transforming health and wellness through patient-centered, team-based medical practice.”
Learn more at: https://www.aapa.org/about/what-is-a-pa/
Social worker
The profession of social work aims to improve functioning and overall well-being within individuals, families, organizations, and communities through change efforts. With a focus on the poor, the oppressed, and the vulnerable, social sciences such as sociology, psychology, political science, public health, economics, law, community and organizational change, are applied. Needs assessments are completed and interventions are planned to solve personal and social problems within client systems to enhance social change. Social work practice is often divided into three levels. Micro-work involves working directly with individuals and families, such as providing individual counseling/therapy or assisting a family in accessing services. Mezzo-work involves working with groups and communities, such as conducting group therapy or providing services for community agencies. Macro-work involves fostering change on a larger scale through advocacy, social policy, research development, nonprofit and public service administration, or working with government agencies. Professional training requires a master’s degree and most states require professional licensure. Social Workers are employed in a variety of settings including healthcare, government agencies education, corrections, public health, and public policy.
Source: Wikipedia
Speech language pathologist
Speech-language pathologists (SLPs) work to prevent, assess, diagnose, and treat speech, language, social communication, cognitive-communication, and swallowing disorders in children and adults.
Learn more at: https://www.asha.org/Students/Speech-Language-Pathology/
THE PUBLIC HEALTH EDUCATOR/PATIENT EDUCATOR’S ROLES AND RESPONSIBILITIES
The U.S. Department of Labor – Bureau of Labor Statistics (BLS) has a classification of health educator and defines health educators (SOC 21-1091) as those that provide and manage health education programs that help individuals, families, and their communities maximize and maintain healthy lifestyles.Health Educators collect and analyze data to identify community needs prior to planning, implementing, monitoring, and evaluating programs designed to encourage healthy lifestyles, policies, and environments.
They link health systems, health providers, insurers, and patients to address individual and population health needs. They may serve as resource to assist individuals, other health professionals, or the community, and may administer fiscal resources for health education programs.
Responsibilities/competencies of CHES
https://assets.speakcdn.com/assets/2251/hespa_competencies_and_sub-competencies_052020.pdf
- Area I: Assessment of Needs and Capacity
- Area II: Planning
- Area III: Implementation
- Area IV: Evaluation and Research
- Area V: Advocacy
- Area VI: Communication
- Area VII: Leadership and Management
- Area VIII: Ethics and Professionalism
CHES in healthcare
Individuals who hold the CHES® and MCHES® certifications have versatility and skillsets to practice in many different career settings, across the country and even overseas. Job settings were identified in the Health Education Specialist Practice Analysis (HESPA) include the following: Community/non-profit, Healthcare/Hospitals, Government, School Health, Academia/Universities, and Business/Worksite. Job titles in the hospital and healthcare sector can vary. Some common titles include Community Benefits Manager, Outreach Manager, Patient Educator or Program Manager, Patient Navigator, Wellness Coordinator, and Health Educator. Health Education Specialists in the Health Care setting may perform the following duties:
- Deliver and assess health education programs
- Coordination and outreach
- Enrollment and initial health assessments
- Motivate others to initiate behavior change
- Communicate/liaise with primary care physicians, hospitals and other health care providers
- Plan for health education interventions
- Translate medical and health education material for dissemination to client/patient