Doctorate in Athletic Training online
A.T. Still University’s (ATSU) Doctor of Athletic Training (DAT) program develops clinical and academic leaders who advance the athletic training profession. Doctors of athletic training serve as expert clinicians, educators, and administrators with advanced knowledge and skills for analyzing, developing, and implementing practical solutions to improve the delivery of athletic healthcare and the health outcomes of physically active individuals and their communities.
Most athletic trainers who are best fit for an online athletic training doctoral degree are elite clinical, educational, and industry professionals who gain a powerful educational benefit as students are embedded in a work setting while progressing through the curriculum. Educators are prepared with the advanced graduate training needed to effectively teach their own students to succeed as athletic trainers. This doctorate in athletic training program will enable DAT students to apply lessons immediately, while also bringing their unique needs and challenges into the online coursework.
Online Flexibility +
1-Week on-site institute
Customizable:
4 concentration options
Graduate in as
few as 3 years
Applied research
project
industry-renowned
faculty
4 start dates
per year
Graduates gain expertise:
Athletic training doctorate students and alumni
The convenience of online learning, combined with the opportunity to apply lessons immediately to the work setting, is how students are advancing their practice while progressing toward ATSU’s doctor of athletic training degree.
Explore more with AT Life Moments.
Discover from our students and alumni how our DAT degree is different:
See what our DAT students and professors had to say at our Winter Institute event:
Program essentials
Doctor of Athletic Training program online curriculum overview
ATSU’s Doctor of Athletic Training program online curriculum is built at the PhD level of critical thinking and tailored to real-world application. Faculty are industry experts highly familiar with emerging trends in athletic training practice and education.
ATSU-ASHS also offers a post-professional Master of Science program online.
ATSU’s doctor of athletic training degree curriculum is meticulously designed to prepare clinical and academic leaders. Students earning a Doctor of Athletic Training are able to apply lessons immediately, while also bringing their unique needs and challenges into the online coursework.
Learn more about how this curriculum from a leading health sciences University makes a unique difference in helping students advance their knowledge and their careers to the forefront of the athletic training profession.
TOTAL REQUIRED CREDIT HOURS: 69
Program Overview Curriculum Outline
*Eligible for advanced standing, Course also included within the certificate (C) or Master’s (M) program of study
Graduate certificates
Obtain a graduate certificate for enhanced knowledge in your selected area of interest. Upon deciding later to obtain a doctorate degree in athletic training at ATSU, these graduate certificates will provide advanced standing.
Graduate Certificate in Clinical Decision-Making
Outcome:
Demonstrate contemporary knowledge and understanding of leading practices in curricular design, instructional delivery, and assessment in athletic training education.
Objectives:
- Implement quality improvement strategies to identify and address quality gaps for the purpose of improving patient outcomes, system performance, and professional development.
- Demonstrate advanced clinical decision-making in athletic training practice in a manner that integrates clinical experience, patient values, and the best available evidence.
- Demonstrate knowledge of the principles of clinical outcomes assessments and the value of these outcomes to informing patient care and advancing the athletic training profession.
- Utilize information and technology to improve the quality of patient care, manage knowledge, mitigate error, and support clinical decision-making in athletic training practice.

Graduate Certificate in Rehabilitation
Outcome:
Demonstrate advanced practice athletic training knowledge and skills in the specialty area of rehabilitation.
Objectives:
- Integrate the basic science of connective tissue healing (anatomy, physiology, morphology, histology, and biomechanics) into the management of musculoskeletal injuries.
- Demonstrate advanced practice knowledge and skills in the assessment and diagnosis of movement dysfunction.
- Develop advanced practice knowledge and skills in rehabilitation of movement dysfunction through corrective exercise.
- Demonstrate advanced practice knowledge of transitioning from rehabilitation to sport performance.

Graduate Certificate in Orthopaedics
Outcome:
Demonstrate advanced practice athletic training knowledge and skills in the specialty area of orthopaedics.
Objectives:
- Demonstrated advanced practice knowledge and skills in the diagnoses of orthopaedic conditions.
- Demonstrated advanced practice knowledge and skills in the management of orthopaedic conditions
- Demonstrate advanced practice knowledge and skills in the application and interpretation of common imaging and laboratory techniques used in the examination of orthopaedic patients.
- Demonstrate advanced practice knowledge of common orthopaedic surgical procedures with special emphasis on subsequent rehabilitation considerations.

Graduate Certificate in Athletic Training Education
Outcome:
Debate and apply contemporary knowledge and skills in athletic training education.
Objectives:
- Analyze and debate contemporary issues in athletic training education.
- Examine and apply best practices in clinical education and mentoring of athletic training students, young professionals, residents, and fellows.
- Apply instructional delivery and assessment best practices to develop innovative learning opportunities in athletic training
- Apply innovative curricular design best practices to develop an educational offering (eg, professional development, preceptor training, clinical experience) related to athletic training

Graduate Certificate in Sports Neurology and Concussion
Outcome:
Demonstrate advanced practice athletic training knowledge and skills in the sub-specialty area of sports neurology and concussion.
Objectives:
- Integrate the basic science of neurologic injury and tissue healing into the management of neurologic injuries.
- Demonstrate advanced knowledge in the recognition, assessment, management and referral of patients with sport-related neurologic conditions.
- Debate current issues related to the recognition, assessment, and management of activity-related traumatic brain injuries.
- Analyze current concepts regarding the assessment, management, and referral of patients with comorbid disorders who suffer activity-related traumatic brain injury.
Requirements
The DAT program will admit athletic training professionals with diverse professional and personal experiences who have demonstrated capacity to pursue a rigorous course of graduate study. Prospective students will be selected by considering the overall qualities of the applicant through application content, academic record, and prior experience.
Candidates accepted for admission must demonstrate and/or submit documentation of the following prior to matriculation:
Candidates accepted for admission to the DAT program will have earned a masters or higher degree from a regionally accredited institution. Applicants must submit official transcripts from college/university where the highest degree was earned.
Applicants to the Athletic Training program must demonstrate Board of Certification (BOC) certification as an athletic trainer or substantial equivalence, such as credentialing from the Canadian Athletic Therapist Association, Athletic Rehabilitation Therapists of Ireland, Society of Sports Therapists, British Association of Sport Rehabilitators and Trainers. Verification of progress toward completion of all eligibility requirements to sit for the BOC certification examination will be accepted at the time of application, but BOC certification must be verified prior to matriculation.
Students must demonstrate proof of state licensure (if required in your current state of residence). A photocopy of a current state license is acceptable.
Candidates must have achieved a minimum overall graduate cumulative GPA of 2.75 (on a 4.0 scale).
One official recommendation form must be completed by an academic advisor, professor, employer, or other individual who can attest to the applicants potential for success in the doctoral program. Letters from an educational consulting service will not qualify. Recommendations must be submitted for each application year.
Candidates are expected to be computer literate and experienced in word processing. All curricula require extensive computer usage. Accepted applicants are required to have a personal computer prior to matriculation and have access to a high-speed Internet connection.
Candidates must submit an application form.
GRE scores are not required for admission to the DAT.
Applicants are required to demonstrate proficiency in English when applying to the Arizona School of Health Sciences, A.T. Still University. Written and spoken proficiency in the English language may be demonstrated by one of the following options:
- Option 1 - English is your first language.
- Option 2 - Graduated from a regionally accredited four year university or college in the United States (minimum BA or BS).
- Option 3 - You are demonstrating your English proficiency by submitting acceptable scores on the Test of English as a Foreign Language (TOEFL) or the International English Testing Service (IELTS).
Acceptable minimal scores for ASHS applications are:
- Internet based total score = 80
- Acceptable IELTS score are an overall band score of 6.5
The TOEFL is administered by TOEFL/TSE Services, P.O. Box 6151, Princeton, NJ, 08541-6151, USA 609. 771.7100. Information is available at www.toefl.org. A.T. Still University’s institutional code is 0339. Please be sure to include this information when you submit your application packet. TOEFL Educational Testing Services P.O. Box 6151 Princeton, NJ 08541-6151 609.771.7100
Candidates must complete a phone interview with the program director.
Licensure
Students must demonstrate proof of state licensure (if required in your current state of residence). A photocopy of a current state license is acceptable.
Technology Requirements
All ATSU students are required to own a computer system.
Program Outcomes
Upon completion of the Doctor of Athletic Training program at ATSU, students will be able to achieve the following outcomes:
- Demonstrate advanced clinical decision-making to determine the effectiveness of athletic training practice.
- Demonstrate advanced knowledge and skills in orthopaedic rehabilitation
- Demonstrate an understanding of the characteristics of professional leadership, and evaluate and influence health policy and delivery systems, especially in the provision of athletic healthcare services.
- Produce an applied research project that addresses a significant clinically oriented issue relevant to athletic training practice.
Clinical Decision-Making Foundation/Certificate Program
- ATRN 7110: Quality Improvement and Patient Safety* (C)(M)
- ATRN 7120: Evidence-Based Practice* (C) (M)
- ATRN 7130: Patient-Oriented Outcomes* (C) (M)
- ATRN 7140: Health Information Technology* (C)
*Eligible for advanced standing, Course also included within the certificate (C) or Master’s (M) program of study

ATRN 7110: Quality Improvement and Patient Safety* (C)(M)
Quality improvement is the consistent, combined effort of many to make changes in healthcare that will improve patient outcomes, system performance, and professional development. This course is designed to enhance the athletic trainer’s understanding of quality improvement, especially as it relates to patient outcomes (health), system performance (care), and professional development (learning). An overview of the history of quality improvement in healthcare will be provided to provide a global understanding of the value of quality improvement to the advancement of patient care. Additionally, the Model of Improvement will serves as the theoretical foundation for the course. Topics will include creating and managing interprofessional teams, identifying quality improvement issues, process literacy, data collection for continuous improvement, and implementing system changes. During the course, students will also be introduced to common tools used in quality improvement projects, such as process diagrams, cause-and-effect diagrams, run charts, and plan-do-study-act cycles. Achievement of course learning objectives will occur through readings, multi-media presentations, discussions, presentations, and individual and/or group assignments.

ATRN 7120: Evidence-Based Practice* (C) (M)
This course is designed to enable the athletic trainer’s clinical decision-making process in a manner that integrates clinical experience, patient values, and the best available evidence. It is also intended to build on entry-level evidence-based practice courses with the use of informatics and technology to access the medical literature. The course will cover advanced topics related to the EBP process, framing clinical questions to enhance clinical decision-making, searching the literature, critical appraisal, integration and evaluation of the evidence, grading levels of evidence and strength of recommendations, patient values, and statistical terminology related to EBP.

ATRN 7130: Patient-Oriented Outcomes* (C) (M)
Advanced Patient-Oriented Outcomes is designed to enhance the athletic trainer’s ability to employ clinician-based and patient-based clinical outcome measures for the determination of effective clinical decision-making through the practice of providing patient-centered whole person healthcare. Discussion of disablement models and outcomes research as the foundations to evidence-based practice will be provided. The use of disablement models as a framework for whole person healthcare and the evaluation of health-related quality of life will be presented. This course builds upon the basic components of clinical outcomes assessment by providing advanced content related to clinician- and patient-oriented outcomes. Instruction on the selection, implementation, and use of single- and multi-item, general and specific patient-rated outcomes instruments will be given. Details regarding the concepts of measurement properties, including assessment of measurement change, will be provided. Opportunity to develop an outcomes study through creation of a clinical question in PICO format will be provided and discussion of using practice-based research networks as means to conducting outcomes investigations will occur.

ATRN 7140: Health Information Technology* (C)
The purpose of this course is to provide the athletic trainer with a survey of relevant concepts, tools, and systems of healthcare informatics and technology that may be useful throughout the clinical decision-making process. An understanding of informatics concepts and skills related to the use of technology has been identified as critical for all modern healthcare professionals. Moreover, informatics and technology provide several distinct advantages to the modern healthcare system, including, but limited to: cost savings; error detection; quality improvement, and; improved patient outcomes.
Innovation/Winter Institute

ATRN 8140: Leadership and Professionalism in Athletic Training
This course offers an examination and application of theories of professionalism and leadership as they related to various aspects of the practice of athletic training. Topics include, but are not limited to: Contemporary leadership theories, Medical professionalism, Organizational communication, Personal effectiveness and productivity, Communities of practice, Leading change, and Conflict management. The course requires students to be active participants in the learning process. We will rely on a series of readings (eg book chapters, classic and contemporary articles, research studies), presentations, discussions, and both reflective and authentic applied assignments to provide a deeper understanding of leadership and professionalism and their impact the athletic training profession. By the end of this course you should have the foundational knowledge and a framework for action that will allow you to make informed decisions about your own leadership roles and pursue meaningful change in both your work setting and your profession.

ATRN 8150: Winter Institute – Innovation to Advance Athletic Health Care
The four-day intensive Winter Institute is focused on Innovation to Advance Athletic Health Care. The thread of innovation is woven throughout the course with particular emphasis on innovation to advance higher education, innovation to advance patient care, and innovation to advance research. This course is designed to promote in-depth interaction between students and faculty to facilitate the development of action plans for leading innovation in athletic health care education, patient care, and research. Students will prepare a project proposal specific to their work environment to help them develop the knowledge and skills for leading innovations within their own health care facilities and institutions. The Institute faculty consists of leading innovators in athletic health care from across the country that students will have the opportunity to learn with and from. Each faculty member will lead educational sessions in their respective area(s) of expertise and will serve as small group facilitators. Students will be mixed throughout the week into three distinct small groups that meet daily, each facilitated by an internal (ATSU) and external faculty member, to maximize opportunities for extensive interactions with peers and faculty. Study sections will be used at the beginning of each day to stimulate critical thinking and promote dialogue around the theme of the day. Project groups will meet daily to help students develop their innovative projects for leading and managing environmental change. Reflection groups will meet at the end of each day to discuss the days key points, where students experienced their greatest knowledge gains, how the information can be translated into their work setting, and what new questions may have emerged. An extensive course-reading list will be provided in advance of the face-to-face meeting and students will be required to read all course material prior to the educational sessions. In addition to the project proposal, readings, and attending the face-to-face sessions, students will be expected to complete a post-Institute assessment.

Applied Research Foundation
- ATRN 8010: Research Methods & Design * (M)
- ATRN 8020: Methods of Data Analysis* (M)
- ATRN 8100: Practice-Based Research
- ATRN 9001: Analyzing the Problem
- ATRN 9002: Proposing a Solution
- ATRN 9003: Implementing and Evaluating the Solution
- ATRN 9004: Completing and Disseminating the Project
*Eligible for advanced standing, Course also included within the certificate (C) or Master’s (M) program of study

ATRN 8010: Research Methods & Design * (M)
This course will focus on the development and application of graduate level knowledge and skills related to research methods in health sciences. Skills regarding the development of a research proposal, including the identification of a problem, conducting a literature review, developing a hypothesis, designing a study and submitting an Institutional Review Board application are integral components of this course.
ATRN 8020: Methods of Data Analysis* (M)
This course will focus on development and application of graduate level knowledge and skills related to the use of statistical methodology in health sciences research.

ATRN 8100: Practice-Based Research
This course aims to improve the athletic trainer’s understanding of and, ability to conduct, practice-based research. Practice-based research represents the last step of the transnational research continuum and is vital to the translation of evidence into routine clinical practice. In brief, practice-based research is conducted by clinicians at the point-of-care, with real patients, and during the usual course of patient care. To meet its purpose, this course will cover fundamental concepts related to practice-based research including but not limited to the clinician-scientist model, researcher-clinician partnerships, common study designs and statistical approaches, implementation and dissemination of evidence, and practice-based research networks.

ATRN 9001: Analyzing the Problem
This course is the first in a series of four courses designed to assist you with the development of an applied research project (ARP) through the stages of reviewing the literature to project dissemination. Understanding the past and current literature around your desired research topic area is crucial to the development of a sound research project. Therefore, the purpose of this course is to provide you with the knowledge and skills to successfully review the literature around your chosen ARP topic and write a focused review of literature, which will serve as a foundational paper for your ARP.
ATRN 9002: Proposing a Solution
This course is the second in a series of four courses designed to assist you with the development of an applied research project (ARP) through the stages of reviewing the literature to project dissemination. The purpose of this course is to provide you with the knowledge and skills to develop and present the proposal for your required ARP. The proposal is crucial for the success of your ARP, as it describes in detail the research questions, hypotheses, and methodological details of your study.
During this course you will work closely with your ARP advisor to ensure your ARP proposal is methodologically sound and feasible. By the end of this course, you will have completed your ARP proposal and will present your project to your ARP advisor and submit your application to the IRB.
ATRN 9003: Implementing and Evaluating the Solution
This course is the third in a series of four courses designed to assist you with the development of an applied research project (ARP) through the stages of reviewing the literature to project dissemination. The purpose of this course is to provide you with the knowledge and skills to continue to finalize your data collection forms and sampling methodology and to successfully complete your data collection as well as properly manage your data. Additionally, this course will help you to develop and implement an analysis plan for your ARP, based on previous methodological and statistical courses, and write the bulk of your results section so that you will be ready to complete your manuscript and prepare it for dissemination in the next course.
ATRN 9004: Completing and Disseminating the Project
This course is the fourth and final course in a series of four courses designed to assist you with the development of an Applied Research Project (ARP) through the stages of reviewing the literature to project dissemination. The purpose of this course is to provide the knowledge and skills needed to successfully complete your ARP manuscript, and to identify possible strategies for the dissemination your research findings through means, such as poster and oral presentations or manuscript submission.

Rehabilitation Track/Certificate Program
- ATRN 7210: Foundations of Tissue Healing
- ATRN 7230: Assessment of Movement Dysfunction
- ATRN 7240: Corrective Techniques for Movement Dysfunction
- ATRN 7250: Rehabilitation Considerations for Sport Performance
*Eligible for advanced standing, Course also included within the certificate (C) or Master’s (M) program of study

ATRN 7210: Foundations of Tissue Healing
This course is designed to enhance the athletic trainers’ ability to plan and implement a comprehensive sports injury rehabilitation program based on the sequential biological events of connective tissue healing. Orthopaedic basic science concepts involved in clinical assessment, establishment of therapeutic objectives, and selection of therapeutic agents will be addressed. The histology, morphology, and biomechanics of soft connective tissues, muscle, articular cartilage, and peripheral nerves will be presented. Subsequently, the basic science of tissue healing following injury will be covered. Special focus is placed on the relationships between tissue healing physiology and selection of appropriate therapeutic interventions. Current topics in soft tissue healing and rehabilitation, including viscosupplementation, graft ligamentization, and biologic treatment techniques will be discussed. This course provides the orthopaedic basic science foundation for discussion of therapeutic techniques in future rehabilitation courses.

ATRN 7230: Assessment of Movement Dysfunction
This course introduces and explores the foundational concepts of structure and function as they relate to fundamental patterns of human movement. Neuro-developmental progression, motor development, motor learning, and motor control concepts will be presented. Utilizing dynamic systems theory and tensegrity models, factors contributing to movement dysfunction will be identified and techniques for movement assessment will be outlined and discussed. Following the completion of this course, students will be able to demonstrate advanced knowledge and skills in the assessment and diagnosis of movement dysfunction

ATRN 7240: Corrective Techniques for Movement Dysfunction
This course provides the athletic trainer with advanced knowledge in the rehabilitation of orthopaedic injuries, by utilizing corrective techniques to restore movement patterns and function. Emphasis is placed on integration of tensegrity and dynamic systems models to develop a sequential and progressive rehabilitation program, centered on restoration of movement patterns in fundamental, transitional, and functional postures. Concepts of mobility, sensorimotor control, movement patterning, and neurodevelopmental progression will be studied. Assisted, active, and reactive techniques for improving mobility, stability, and movement will be taught.

ATRN 7250: Rehabilitation Considerations for Sport Performance
This course provides the athletic trainer with the advanced knowledge on how to bridge the gap from rehabilitation to sport performance. Neuromuscular considerations such as psychomotor and somatosensory control will be explored. Considerations for strength training, time under tension, power development and athletic movement prescription will be examined. Following this course, the athletic trainer will be able to develop a comprehensive program for the athlete who is returning to sport post-injury.

Orthopaedics Track/Certificate Program
- ATRN 7410: Orthopaedic Diagnostic Evaluation
- ATRN 7430: Orthopaedic Imaging and Labs
- ATRN 7440: Orthopaedic Surgical Considerations
- ATRN 7420: Orthopaedic Management
*Eligible for advanced standing, Course also included within the certificate (C) or Master’s (M) program of study
ATRN 7410: Orthopaedic Diagnostic Evaluation
This course is designed to provide the athletic trainer with advanced knowledge and clinical skills in the pathology, examination, and diagnosis of orthopaedic and sport-related injuries to the upper and lower extremities, the back, and spine. Content is presented with an emphasis on integrating evidence-based practice principles to enhance the student’s clinical decision-making skills in injury evaluation and diagnosis. Focus will be placed on developing clinical reasoning skills to enhance the student’s ability to accurately and efficiently utilize the physical examination and diagnostic tests to evaluate complex orthopaedic conditions, recognize atypical presentations, identify non-orthopaedic conditions that present as orthopaedic conditions, and recommend and interpret appropriate imaging and laboratory tests. Students will engage in weekly collaborative learning activities and independent assignments to enhance their clinical skills in Orthopaedic Diagnostic Evaluation.
ATRN 7430: Orthopaedic Imaging and Labs
This course is designed to enhance the athletic trainer’s knowledge regarding common imaging and laboratory techniques used in the management of orthopaedic patients. Students will be exposed to various imaging modalities including radiographs, magnetic resonance imaging, CT scans, and musculoskeletal ultrasound. The use of laboratory tests for injury and illness will also be examined. Students will engage in weekly collaborative learning activities and independent assignments to evaluate the sensitivity and utility of imaging and laboratory tests used in athletic health care.
ATRN 7440: Orthopaedic Surgical Considerations
This course is designed to enhance the athletic trainer’s knowledge and awareness of special considerations for rehabilitation following common orthopaedic surgeries. The course focuses on improving the athletic trainer’s ability to provide quality education and counseling to their orthopaedic patients through the development of advanced knowledge and skills in post-surgical rehabilitation. Surgical techniques for common orthopaedic conditions of the upper and lower extremities will be presented. Tissue response to surgery, post-surgical rehabilitation guidelines and timelines, and surgical outcomes will be discussed. Students will engage in weekly collaborative learning activities to critically appraise the current evidence for post-surgical rehabilitation approaches. The course culminates with the development of a comprehensive, evidence-based post-surgical rehabilitation protocol for an orthopaedic surgery of the student’s choice.

ATRN 7420: Orthopaedic Management
This course is designed to enhance the athletic trainers’ ability to effectively manage patients with increasingly complex orthopaedic conditions. Content focuses on management of complex orthopaedic conditions with and without co-morbidities and includes the development prioritized care plans, strategies to maximize long-term health related quality of life, identifying criteria and plans for safe return to participation and to maximize sports performance, engaging in patient education. Students will engage in weekly collaborative learning activities and independent assignments to enhance their clinical skills in Orthopaedic Management.

Athletic Training Education Track/Certificate Program
- ATRN 8160: Contemporary Issues in Athletic Training Education
- ATRN 8170: Applied Clinical Education and Mentoring
- ATRN 8180: Instructional Delivery and Assessment in Athletic Training
- ATRN 8190: Programmatic Planning and Curricular Design in Athletic Training
*Eligible for advanced standing, Course also included within the certificate (C) or Master’s (M) program of study

ATRN 8160: Contemporary Issues in Athletic Training Education
This course that will explore contemporary issues in athletic training education, with special emphasis on the continuum of education from professional programs through residency and fellowship training to post-professional degree programs, such as the Doctor of Athletic Training and Doctor of Philosophy degrees, as well as continuing education and maintenance of competence. A global perspective of the structure of health professions education, accreditation, and current issues in higher education will be explored. Students will develop insights and discuss implications for the ever-changing nature of health professions education, with a focus on contemporary issues in athletic training education.

ATRN 8170: Applied Clinical Education and Mentoring
This course is intended to improve the student’s understanding and application of best practices in clinical education and mentoring in athletic training professional education and residency/fellowship training programs. Focus will be on best practices regarding bridging the gap between didactic and clinical education, clinical education techniques and models, preceptor mentoring, and student/resident/fellow mentorship models. Focused discussion regarding developing assessment activities at the point-of-care to facilitate practice-based research is included. Contemporary issues in clinical education, facilitating transition to practice, and mentoring within the health professions will also be presented.
ATRN 8180: Instructional Delivery and Assessment in Athletic Training
This course focuses on applying instructional delivery and assessment best practices to develop innovative learning opportunities in the field of athletic training. Students will gain a comprehensive understanding of emerging teaching and learning theories in athletic training, while exploring the contemporary use of educational technology to enhance student learning. Additionally, students will gain knowledge on the student competence continuum and the characteristics of learners at each level, enabling them to tailor their instructional methods and assessments to meet the diverse needs of learners.

ATRN 8190: Programmatic Planning and Curricular Design in Athletic Training
This course is designed to prepare aspiring and current athletic training educators and preceptors to deliver high-quality educational opportunities. Emphasis will be placed on the principles and practices of programmatic planning and curricular design in athletic training. Students will explore instructional design theories and techniques, develop learning outcomes and objectives, design effective learning activities, select appropriate assessments, and evaluate and improve curricular offerings. Through a combination of theoretical exploration and practical application, students will develop the knowledge and skills necessary to create and enhance educational programs in the field of athletic training.

Sports Neurology and Concussion Track/Certificate Program
- ATRN 7310: Foundations of Sport Neurology
- ATRN 7320: Diagnosis and Management of Neurologic Conditions in Sport
- ATRN 7330: Classification and Management of Traumatic Head Injury
- ATRN 7340: Assessment and Management of Complex Patients with Concussion
*Eligible for advanced standing, Course also included within the certificate (C) or Master’s (M) program of study

ATRN 7310: Foundations of Sport Neurology
This course is designed to enhance the athletic trainers’ ability to manage neurological injuries resulting from participation in sports and physical activity. Basic science concepts regarding neurological mechanisms of pain, pathophysiology of neurologic injuries, neurodynamics, and the psychological contributions of pain will be discussed. This course will serve as a foundation to the other courses in the Sports Neurology and Concussion track or graduate certificate program.

ATRN 7320: Diagnosis and Management of Neurologic Conditions in Sport
This course is designed to enhance the students’ knowledge and skills regarding the recognition, assessment, management, and referral of patients who present with neurologic conditions. Specific attention will be placed on understanding red flags for various conditions, diagnostic testing, and appropriate care for various conditions. The course will use a mix of online readings, videos, and discussion forums to foster collaboration among students.

ATRN 7330: Classification and Management of Traumatic Head Injury
This course is designed to expand the student’s understanding of traumatic head injury. The course will span the spectrum of head injury from catastrophic head injury with internal hemorrhage to mild traumatic brain injury or concussion. Specifics regarding assessment, treatment, and management will be presented. The course will use a mix of online readings, videos, and discussion forums to foster collaboration among students.

ATRN 7340: Assessment and Management of Complex Patients with Concussion
This course will provide a thorough examination of the treatment of patients with complex medical concerns who suffer a concussion. Specific attention will be focused on the patient’s past medical history and co-morbid factors and how these may influence the assessment, treatment, and management of head injuries. The course will use a mix of online readings, videos, and discussion forums to foster collaboration among students.
Tuition
Review tuition and fees for the Doctor of Athletic Training Degree program. Please note tuition and fees are subject to change.
Student Technology Fee: This fee is charged to ATSU students to recover, in whole or in part, the costs of providing and maintaining technology services to students that include, but need not be limited to: access to Gmail and the g-suite of products, Canvas and other learning platforms and software, help desk services, and computer and multimedia work stations and laboratories.
Financial Services
For information on financial aid, visit ATSU’s Enrollment Services or contact them at 660.626.2019 or enrollmentservices@atsu.edu.
Tamara C. Valovich McLeod, PhD, ATC, FNATA, is the Athletic Training program director, professor of Athletic Training, research professor in the School of Osteopathic Medicine in Arizona, and the John P. Wood, DO, endowed chair for Sports Medicine at A.T. Still University in Mesa, Arizona.
Dr. McLeod completed her doctor of philosophy degree in education with an emphasis in sports medicine from the University of Virginia. She is the founding director of the Athletic Training Practice-Based Research Network. Her research has focused on the pediatric athlete with respect to sport-related concussion. Her current work is investigating the short- and long-term effects of pediatric sports concussion as well as recovery following concussion on traditional concussion assessments, academics, and health-related quality of life.
Dr. McLeod is also involved with pediatric sports injury education and prevention through the Positive Play Project in conjunction with Mesa Parks and Recreation.
Dr. McLeod was a contributing author for the NATA Position Statement on the Management of Sport-Related Concussion, the lead author on the NATA Position Statement on the Prevention of Pediatric Overuse Injuries, and a consultant and contributing author on the Appropriate Medical Coverage for Secondary School-Aged Athletes. Dr. McLeod serves on numerous editorial boards, and publishes frequently in the athletic training and sports medicine journals and is a NATA Fellow.
Dr. Anderson is a Tenured Professor in the ATSU Athletic Training programs. He teaches a variety of courses in both the online DAT and MSAT programs, with a focus on developing clinical skills and athletic training clinical education Dr. Anderson also advises doctoral applied research projects in the DAT program. Dr Anderson holds a Level 1 Functional Movement Screen™ certification, and is an accredited Graston Technique™ clinician. He has extensive experience and training in therapeutic exercise prescription, fundamental movement patterns, and manual therapy techniques.
Prior to coming to ATSU, Dr. Anderson worked full-time clinically for 10 years as an athletic trainer in the collegiate, high school, and clinical settings. Dr. Anderson's research interests include the assessment and correction of fundamental movement patterns, the development of clinical reasoning skills and advanced clinical practice, and athletic training clinical education. Dr. Anderson is the Chair of the CAATE Standards Committee, and a member of the CAATE Professional Accreditation Council. He is also a member of the Association for Athletic Training Education (AATE) Research Network, and serves as a member of the editorial board for the Journal of Sport Rehabilitation. Dr. Anderson earned his Bachelor’s of Science in Sports Medicine and Athletic Training from Missouri State University, his Masters of Science in Sports Health Care from A.T. Still University, and his Doctor of Health Science degree from Nova Southeastern University. He has been recognized as the Arizona School of Health Sciences Educator of the Year (2016), Distinguished Service of the Year (2019), and Scholar of the Year (2021); named a Distinguished Educator by the RMATA in 2019, and received the NATA Service Award in 2018.
Cailee E. Welch Bacon, PhD, ATC, FNATA is professor in the Department of Athletic Training Programs and a research professor in the Department of Basic Science in the School of Osteopathic Medicine in Arizona at A.T. Still University. Dr. Bacon earned her bachelor of science degree in athletic training from Boston University, followed by a master of science in education degree in athletic training from Old Dominion University. She also earned her doctor of philosophy degree in human movement science with a focus in athletic training curriculum and instruction from Old Dominion University, where she investigated the effectiveness of educational techniques to aid athletic trainers in learning the fundamentals of evidence-based practice. Dr. Bacon completed a post-doctoral research fellowship within the Center for Clinical Outcome Studies at A.T. Still University, which focused on patient-oriented outcomes. Dr. Bacon serves as an Associate Editor for the Journal of Athletic Training Editorial Board and the Athletic Training Education Journal, and is a contributing scholar for the Association for Athletic Training Education Research Network. Dr. Bacon also serves as the Associate Director for the Athletic Training Practice-Based Research Network (AT-PBRN), where she primarily oversees the continuing education platform and the cost-free academic electronic medical record (AEMR). Dr. Bacon’s research agenda seeks to understand how the educational outcomes of health professions education programs shape and guide the practice patterns of healthcare professionals. The long term goal of her research is to determine key elements that drive the successful educational outcomes of professional and post-professional athletic training programs to ensure future generations of athletic trainers are able to effectively provide athletic training services to enhance patient outcomes and reduce healthcare costs. In 2023, Dr. Bacon was named a Fellow of the National Athletic Trainers’ Association.

Sue Falsone, PT, DPT, MS, SCS, ATC, L-AT, CSCS, COMT, RYT, is an associate professor in ATSU-ASHS Athletic Training program. She teaches courses within the athletic training Master of Science degree program and online courses in orthopaedic rehabilitation foundation within the online Doctor of Athletic Training program. She also serves as a clinician scientist within the school’s Athletic Training Practice-Based Research Network. Dr. Falsone’s many accomplishments include being the first female head athletic trainer in any of the four major American professional sports leagues, when she was named the head athletic trainer for the LA Dodgers in 2012. She also served as the head of athletic training and sport performance for the U.S. Men’s National Soccer Team. She is currently serving as the Director of Movement and Return to Performance for the Houston Texans. She is known internationally for her expertise in sport rehabilitation and performance enhancement and bridging between physical therapy and return to sport. An alumna of Daemen College, Dr. Falsone graduated from the University of North Carolina at Chapel Hill with a master’s degree in human movement science; is owner and founder of Structure and Function Education, an educational company working to bring the concepts, philosophies and techniques of dry needling to the allied healthcare professional.

Dr. Rachel Geoghegan is the newest faculty member in the Department of Athletic Training, joining the faculty in 2023. She brings with her nearly two decades of full-time clinical experience in the college/university setting at locations across the country including Idaho State University, Gonzaga University, and Boston University. As a clinician, she boasts a contemporary clinical expertise in non-orthopedic conditions with a particular interest in female athlete health concerns and pelvic health. She originally hails from South Carolina where she earned a Bachelor of Science degree in Athletic Training from Erskine College in Due West, SC, and a Master of Human Resource Development from Clemson University in Clemson, SC. In 2020, she rounded out her education by earning her Doctor of Athletic Training degree from A.T. Still University. While new to academia, Dr. Geoghegan has experience as a clinical educator by serving as a preceptor for a number of institutions including Idaho State University, Whitworth University, University of Idaho, Washington State University, Boston University, and Chobanian and Avedisian School of Medicine. Dr. Geoghegan is also active in professional service at the local, regional, and national level and seeks to advance the profession any chance she gets. Her research interests include non-orthopedic conditions treated by athletic trainers, pelvic health among athletes, and female athlete health concerns. She is passionate about normalizing compassionate and appropriate conversations about pelvic health between athletic trainers and their patients.

Nicolette “Nikki” Harris serves as an Assistant Professor and the Director of Student Recruitment for the Athletic Training Programs at A.T. Still University. An alumnus of the ATSU Doctor of Athletic Training (DAT) program, Dr. Harris brings a wealth of clinical experience to this role. Prior to arriving to ATSU, she spent 6 years as the Coordinator for Athletic Training Services for Florida International University (FIU) where she worked to enhance the health care services provided to both FIU students and campus recreation participants. In addition, she served 3 years as the Head Athletic Trainer at Miami Booker T. Washington Senior High school providing care to secondary school athletes during their pursuit of 4 State Championship Titles.
In addition to her clinical practice, she has served as a Clinical Assistant Professor and Clinical Preceptor to athletic training students. Nikki actively engages in professional service at all levels, currently sitting as the NATA Career Advancement Committee (CAC) Chair Elect, the BOC Liaison to the Athletic Training Research Agenda Committee (ATRAC) as well as a member of the CAATE Education Committee. Dr. Harris values the effects of research on practice and education and has demonstrated a commitment to the advancement of diversity, equity, inclusion, and social justice through her scholarly works.

Kenny Lam, ScD, ATC, FNATA is a professor of clinical research within the Department of Interdisciplinary Health Sciences at A.T. Still University (ATSU). He received a bachelor of science in athletic training and a master of education in human movement from Boston University. He also completed his doctor of science degree from Boston University with a focus on movement sciences. Prior to becoming a faculty member at ATSU, Dr. Lam completed a Post-Doctoral Research Fellowship within the Center of Clinical Outcomes Studies at ATSU with a focus on patient-oriented outcomes research. His current line of research seeks to understand the overall impact of sport-related lower extremity injuries on patient-oriented outcomes such as health-related quality of life. In addition to his faculty responsibilities, Dr. Lam serves as the director of the Athletic Training Practice-Based Research Network (AT-PBRN) and as the vice chair of the Institutional Review Board at ATSU - Mesa campus. He also serves as a member of the Research Committee for the NATA Foundation, a member of the Athletic Training Research Committee of the NATA Foundation, and an editorial board member for the Journal of Athletic Training and Journal of Sport Rehabilitation. In 2022, Dr. Lam was named a Fellow of the National Athletic Trainers’ Association. Prior to earning his doctorate, Dr. Lam practiced as a certified athletic trainer at Boston University, Rutgers University - New Brunswick, and the Massachusetts Institute of Technology.

Alison Snyder Valier, PhD, ATC, FNATA, holds the positions of Professor within the Department of Athletic Training and Assistant Director of Research Support at A.T. Still University (ATSU). She received her bachelor of arts degree in psychology from Whitman College in Washington and a master of science degree in exercise physiology at the University of Toledo in Ohio. In addition, she received her doctorate in exercise science from the University of Toledo, where she majored in applied physiology and completed a minor in human anatomy. Dr. Valier completed a Post-Doctoral Research Fellowship in Clinical Outcomes Research, awarded to her by the NATA Research and Education Foundation. She is actively involved in the instruction of students enrolled in the Post-Professional Masters in Athletic Training and the Doctor of Athletic Training programs at ATSU. Alison's extensive research proficiency encompasses Clinical Outcomes Assessment, with a distinct emphasis on leveraging Patient Reported Outcomes Instruments to facilitate informed clinical decision-making. Her scholarly pursuits also span social determinants of health and their impact on individuals leading physically active lives, epidemiology of athletic injuries, and enhancing healthcare quality. Throughout her career, Alison has demonstrated a dedicated commitment to the advancement of the Athletic Training field. Her contributions include holding pivotal roles such as Chair of the NATA Foundation Pronouncements Committee and membership in the NATA Foundation Research Committee. She has also served as a reviewer for the Journal of Athletic Training, Athletic Training and Sports Health Care, and the Journal of Sport Rehabilitation. Dr. Valier has been recognized for her outstanding contributions to the field of Athletic Training, earning her the distinction of being named a Fellow of the National Athletic Trainers’ Association in 2022.

Kelsey J. Picha, PhD, ATC is an Assistant Professor in the Department of Interdisciplinary Health Sciences where she co-teaches Clinical Anatomy. Dr. Picha has previously taught functional anatomy and assisted with several other courses related to the human body and patient care. Her research interests are in the areas of patient adherence to rehabilitation and social determinants of health in athletic health care. Dr. Picha has secured grant funding both internally and externally for her work. She currently serves on several professional committees including the AACA Branding, Promotion, and Outreach Committee, the NATA Education Advancement Committee, and AZATA Governmental Affairs Committee. Dr. Picha also serves as a section editor for the Clinical Practice in Athletic Training Journal and serves on the editorial board for the Journal of Sports Rehabilitation. Dr. Picha earned her bachelor of athletic training degree from Minnesota State University, Mankato, master of science degree in post-professional athletic training from A.T. Still University, and earned her doctor of philosophy degree in rehabilitation sciences from the University of Kentucky.

Sara Brown is emeritus faculty at Boston University, where she served as the director of the athletic training program and clinical associate professor until her retirement in July 2020. She attended Miami University (BS) and University of Arizona (MS). Beyond her direct experience in professional education, she also served as the as chair of the NATA’s Executive Committee for Education, the chair of the Standards Committee for the CAATE, and on the Board of Directors for the Board of Certification. She is one of the founders of the Association for Athletic Training Education and currently serves as its vice president.

R. Mark Laursen, MS, ATC, was selected as Boston University’s Director of Athletic Training Services in June 2008. At that time, he also was named a Clinical Associate Professor of Athletic Training in BU’s Sargent College of Health and Rehabilitation Sciences. No stranger to BU, Laursen has served in numerous capacities at the University since 1983, when he first joined the Department of Athletics as an assistant soccer coach for two seasons. He has worked as a Clinical Assistant Professor of Athletic Training and is a Faculty in Residence in the Office of Residence Life. Mr. Laursen is an adjunct faculty member for the DAT Winter Institute and has participated since the founding of the program.
From July 2007 to May 2008, he was a clinical instructor at the University of South Carolina. As a member of its graduate faculty, he coordinated all graduate clinical education. Additionally, from 1993-1998 he was the Head Athletic Trainer at Washington College at Chestertown, MD. He has contributed too many publications, has made more than 90 presentations, and is a reviewer for Athletic Therapy Today and The Journal of Athletic Training. He has served as the Treasurer, Vice President and President of the Commission on Accreditation of Athletic Training Education (CAATE). He has visited over 20 schools’ athletic training programs as an Evaluation Team Member or Team Chair for NATA’s Professional Education Committee, CAAHEP and CAATE. He has been awarded Athletic Trainer of the Year from Athletic Trainers of Massachusetts (2013) and NATA’s Head Athletic Trainer of the Year (2007), Service Award (2009) and Most Distinguished Athletic Trainer (2016).
Laursen has volunteered as an Athletic Trainer at numerous sporting events including the Boston Marathon, NCAA championships for men’s basketball, men’s ice hockey and wrestling, and U.S. Figure Skating Challenges. A 1983 graduate of Appalachian State University with a Bachelor of Science degree, Laursen majored in Health Education and minored in Athletic Training. He earned his Master of Science degree in 1986 from Canisius College.

David H. Perrin is Dean of the College of Health and Professor in the Department of Physical Therapy and Athletic Training at the University of Utah. He serves as an adjunct faculty member for the DAT Winter Institute and has been a contributor to the institute since 206.
From 2007 – 2014 he served as Provost and Executive Vice Chancellor at the University of North Carolina at Greensboro and as Dean of the School of Health and Human Performance at UNCG from 2001-2007. Dr. Perrin’s career as an administrator began in 1995 in the Curry School of Education at the University of Virginia where he served as program area director of Kinesiology (then Health and Physical Education). In 1999, he was appointed Chair of the Department of Human Services at UVa. He received his BS in Physical Education from Castleton State College, MA in Athletic Training from Indiana State University, and PhD in Exercise Physiology from the University of Pittsburgh.
Dr. Perrin was editor-in-chief of the Journal of Athletic Training for eight years (1996-2004) and founding editor of the Journal of Sport Rehabilitation (1990-1995). He is author of Isokinetic Exercise and Assessment and Athletic Taping and Bracing, 3nd Edition (with translations in Japanese, Greek, Chinese, Portuguese, Korean and French), editor of The Injured Athlete, Third Edition, and coauthor of Examination of Musculoskeletal Injuries and Research Methods in Athletic Training. He also served as series editor of the 5-textbook Athletic Training Education Series.
For 15 years Dr. Perrin directed the graduate programs in Athletic Training (MEd) and Sports Medicine (PhD & EdD) at the University of Virginia. He was named the Joe Gieck Professor of Sports Medicine, founded the Sports Medicine and Athletic Training Research Laboratory, and mentored over 50 students who received a doctoral degree in Sports Medicine. His primary research interest, funded by the National Institutes of Health, focused on anterior cruciate ligament injury risk factors in female athletes.
From 2007 to 2011 he served on the Advisory Committee on Interdisciplinary, Community-Based Linkages, Bureau of Health Professions of the U.S. Department of Health and Human Services. As a faculty member, he was recipient of a University of Virginia All-University Outstanding Teaching Award in 1997 and in 1998 received the Curry School of Education Foundation’s Outstanding Professor Award. His professional awards from the National Athletic Trainers’ Association include the Sayers “Bud” Miller Distinguished Educator Award in 1996, the Most Distinguished Athletic Trainer award in 1998, the William G. Clancy, Jr., MD Medal for Distinguished Athletic Training Research in 1999, and induction into the Hall of Fame in 2003. In 2015 he received the NATA Research & Education Foundation’s Lifetime Contribution Award. Among his honors are distinguished alumni awards from CSC, ISU, and Pitt, including induction into the Legacy Laureate Society at the University of Pittsburgh in 2008. In 2009 he received an Honorary Doctor of Humane Letters from the Arizona School of Health Sciences at A.T. Still University.

Stacy E. Walker, PhD, ATC is a tenured Associate Professor of Athletic Training at Ball State University. She serves as an adjunct faculty member for the DAT Winter Institute. She has over 30 peer reviewed journal articles, more than 40 professional presentations. Her research agenda focuses on the use of standardized patients to provide additional clinical education experiences for athletic training students and the transition to practice of newly credentialed athletic trainers.
She received the Great Lakes Athletic Trainers’ Association Outstanding Educator Award in 2014. She is an Associate Editor for the Journal of Athletic Training and the Athletic Training Education Journal and is a member of the NATA Research and Education Foundation Research Committee, the Board of Certifications Maintenance of Certification Task Force the Association of Standardized Patient Educators Grants and Research Committee and serves as a CAATE Site visitor. S
he obtained her bachelor of science degree from Southern Illinois University, a masters in rehabilitative science from Clarion University and a masters degree in athletic training from the University of Tennessee at Chattanooga followed by her Doctor of Philosophy degree in administration and teaching from the University of Southern Mississippi.

Andrew P. Winterstein is a clinical professor in the Department of Kinesiology at the University of Wisconsin – Madison where he currently serves as the program director of the athletic training professional preparation program. A graduate of the University of Arizona, University of Oregon, and the University of Wisconsin‐Madison; Dr.Winterstein has been active in athletic training patient care and educational programming at UW‐Madison since 1986. Dr. Winterstein serves as an adjunct professor for the DAT Winter Institute and is the primary course professor for ATRN 8140: Leadership and Professionalism in Athletic Training.
Dr. Winterstein’s academic interests include: emerging technologies and their use in teaching and learning, medical humanities and their application to athletic training education, organizational dynamics, educational interventions/behavioral change, and patient‐reported outcome measures following injury. His papers and abstracts have appeared a variety athletic training and sports medicine journals and he has been privileged to make numerous professional presentations at state, regional, national, and international conferences.
He is the author of three textbooks: The Athletic Training Student Primer (Slack, Inc), Administrative Topics in Athletic Training: Concepts to Practice (Slack, Inc) with Greg Gardner and Gary Harrelson, and The Athletic Trainers Guide to Differential Diagnosis: A Visual Learning Approach (Slack, Inc) co‐authored with Sharon Clark.
Dr. Winterstein has received numerous awards, including the 2016, NATA Most
Distinguished Athletic Trainer Award, 2008 Great Lakes Athletic Training Association Outstanding Educator Award, 2007 Wisconsin Athletic Trainers’ Association Outstanding Educator Award, and the 2006 UW‐Madison School of Education Distinguished Service Award. He and his colleagues are three‐time winners of the NATA Educational Multimedia Committee award for educational innovations and have been awarded the MERLOT Classics Award for exemplary on‐line learning objects.

Dr. Avinash Chandran is the Director of the NCAA Injury Surveillance Program at the Datalys Center for Sports Injury Research and Prevention. Prior to joining the Datalys Center, Dr. Chandran was a Postdoctoral Research Associate in the Department of Exercise and Sport Science at the University of North Carolina at Chapel Hill, where he concurrently worked within the Matthew-Gfeller Sport-Related TBI Research Center, the Center for Study of Retired Athletes, and the Injury Prevention Research Center. Dr. Chandran is a quantitative Epidemiologist, and his research interests are, broadly, in athlete health over the lifespan. Dr. Chandran holds a Bachelor of Science degree in Public Health from the University of Maryland, College Park. He completed his Master of Science in Epidemiology, as well as his PhD in Epidemiology at the George Washington University.

JJ Wetherington, MS, LAT, ATC, BCS-O is a board certified orthopedic specialist athletic trainer. He currently works as a clinical athletic trainer for a fellowship trained sports medicine surgeon at St. Luke's Sports Medicine in Boise, ID. In addition to his clinical duties, he serves as core faculty for St. Luke’s CAATE accredited orthopedic residency program.
His professional career began in 2009 at Flagler College where he provided care for the men’s soccer and baseball teams. In 2014, JJ went on to further his training by completing an orthopedic athletic training residency at St. Luke’s Sports Medicine. Following his residency JJ was recruited to Spectrum Health in Grand Rapids, MI to develop an athletic training residency along with his duties as a clinical athletic trainer. JJ served as program director from 2015-2017. In 2017, JJ returned to St. Luke’s to work clinically and in the operating room specializing in shoulder pathologies. Additionally, JJ is currently adjunct faculty at AT Still University and affiliate faculty at Indiana State University for both of their DAT programs.
Historically, JJ has been the co-leader of the NATA’s Committee on Practice Advancement (COPA) Athletic Trainers in the Physician Practice Workgroup. Currently he serves the athletic training profession as in numerous capacities with many members of the strategic alliance. JJ is currently serving the Commission on Accreditation of Athletic Training Education (CAATE) as as a site visitor for residency programs, previous he has served as a member of the Standards Committee and. He is currently serving the Board of Certification's (BOC) as a member of the Specialty Council. Additionally, for the BOC he has worked on the practice analysis and exam generation of the orthopedic specialty certification. He also is the vice president of the Athletic Trainers in Physician Practice Society (ATPPS).
He has authored and contributed to numerous peer-reviewed and professional publications focusing on athletic training specialization and athletic training residency programs. JJ is a sought-after speaker with multiple presentation nationally on athletic training specialization, improving physician practice efficiencies, and the implementation and utilization of athletic trainers.
JJ earned his bachelor's degree in athletic training in 2007 from Lenoir-Rhyne University in Hickory, North Carolina and a post-professional master's degree in athletic training in 2009 from Indiana University in Bloomington.

Born in Camden, NJ, Brian received a B.A. in physical education with a concentration in sports medicine. Upon graduation from Denison University, he pursued a master’s degree in sports medicine from Ohio University. He continued his post-graduate studies at the Ohio State University where he completed his doctoral degree in Exercise Science.
Dr. Hortz was part of the athletic training staff at Denison University from 1995-2019, he served as the Head Athletic Trainer from 1997-2010, and the Director of Sports Medicine from 2010-2019. His primary responsibilities at Denison University included being a professor in the Department of Health, Exercise, and Sports Studies Major, as well as, directing the sports medicine program. Dr. Hortz has presented at state, national, and international level conferences in different areas focusing on dry needling, athletic training, medical ethics, regulatory issues, health, and physical activity. He served on the Ohio State PTOTAT licensure board for 9 years and has served in many roles from Joint Board Chair, Chair of the AT section, and other board assignments. Dr. Hortz was inducted into the Ohio Athletic Trainers Hall of Fame in 2018 and has received the NATA Service Award in 2015, The Board of Certification Dan Liberia Award in 2009, and was the Ohio Athletic Trainer of the Year in 2008. Included among his professional affiliations are memberships in the National Athletic Trainers Association, the Great Lakes Athletic Association, and the Ohio Athletic Trainers Association.
Dr. Hortz is currently an Instructor and the Director of Research and Education for Structure & Function Education. In addition to his work with Structure & Function Education, he also has a concierge practice and continues to work one-on-one with athletes to make them well.

Chair and Director
Tamara C. Valovich McLeod, PhD, ATC, FNATA, is the Athletic Training program director, professor of Athletic Training, research professor in the School of Osteopathic Medicine in Arizona, and the John P. Wood, DO, endowed chair for Sports Medicine at A.T. Still University in Mesa, Arizona.
Dr. McLeod completed her doctor of philosophy degree in education with an emphasis in sports medicine from the University of Virginia. She is the founding director of the Athletic Training Practice-Based Research Network. Her research has focused on the pediatric athlete with respect to sport-related concussion. Her current work is investigating the short- and long-term effects of pediatric sports concussion as well as recovery following concussion on traditional concussion assessments, academics, and health-related quality of life.
Dr. McLeod is also involved with pediatric sports injury education and prevention through the Positive Play Project in conjunction with Mesa Parks and Recreation.
Dr. McLeod was a contributing author for the NATA Position Statement on the Management of Sport-Related Concussion, the lead author on the NATA Position Statement on the Prevention of Pediatric Overuse Injuries, and a consultant and contributing author on the Appropriate Medical Coverage for Secondary School-Aged Athletes. Dr. McLeod serves on numerous editorial boards, and publishes frequently in the athletic training and sports medicine journals and is a NATA Fellow.

Dean
Dr. Ann Lee Burch is the dean of A.T. Still University’s Arizona School of Health Sciences (ATSU-ASHS). Dr. Burch received her doctor of education from Columbia University, Teachers College in 2005. She received her masters of public health from Columbia University, Mailman School of Public Health in 2002 and her masters of physical therapy from Columbia University, College of Physicians and Surgeons in 1989. She was a postdoctoral fellow with the Research Group on Health Disparities at Teachers College, Columbia University. Her BA is in psychology from the University of Rochester.
Prior to her appointment as dean, Dr. Burch served as vice dean for ATSU-ASHS. She served as the chair of the Physical Therapy Department from 2008-January 2012. Prior to ATSU, Dr. Burch was the director of physical therapy at the University of Puerto Rico, Medical Sciences Campus in San Juan, Puerto Rico. She has held administrative and/or faculty positions at the International Center for the Disabled in NY, NY, Mercy College in NY, and Long Island University in Brooklyn, NY.
Dr. Burch’s area of scholarly interest and application of that interest is in knowledge, attitudes, and self-efficacy of health care providers and healthcare professional students towards underrepresented patient/client groups.
Dr. Burch is the author of a Guide to Physical Therapy (Vault Publishers) which was written to increase information access about physical therapy to both high school graduates and re-entry adults. She was a co-investigator on an NIH grant at the University of Puerto Rico exploring the feasibility of an exercise program for breast cancer survivors living in San Juan. Dr. Burch has lived in Symi, Greece, Taipei, Taiwan, Ahmdebad, India and San Juan, Puerto Rico, and is committed to research, teaching and service that further the understanding of the impact of socioeconomic and cultural variables on health.
She was a member of the class of 2014 cohort of Women in Educational Leadership at Harvard Graduate School of Education. In 2017 she was the co-PI on a Centers for Disease Control, Association for Prevention and Teaching grant exploring a population health case study format for teaching and communicating the impact of social determinants of health on health disparities. She was recently appointed a peer reviewer for the Higher Learning Commission.

Vice Dean
Dr. Salas-Provance, is professor and vice dean of A.T. Still University’s Arizona School of Health Sciences (ATSU-ASHS). Dr. Salas-Provance received her doctorate in speech science from the University of Illinois Urbana-Champaign. She received her masters of health administration from the University of Missouri School of Medicine-Columbia. She holds both a bachelors and masters in Speech Pathology from New Mexico State University.
Prior to her appointment as vice dean, Dr. Salas-Provance served as associate dean of academic and student affairs for the School of Health Professions at the University of Texas Medical Branch Galveston. She served as assistant dean and chair in the College of Education, Department of Special Education and Communication Disorders at New Mexico State University in Las Cruces, New Mexico and department chair in the Department of Communication Sciences and Disorders at the University of Montevallo (AL). She held faculty positions at Fontbonne College and St. Louis University, in St. Louis, MO.
She has made extensive professional contributions to the American, Speech, Language & Hearing Association (ASHA), serving on the Speech-Language Pathology Advisory Council, member of the Financial Planning Board, and the Multicultural Issues Board. She served as coordinator of ASHA’s Special Interest Group (SIG) 14, Communication Disorders and Sciences in Culturally and Linguistically Diverse populations and was a founding member and coordinator of SIG 17, Global Issues in Communication Sciences and Disorders. She is an ASHA Fellow and received ASHA’s highest awards for “Special Recognition in Multicultural Affairs” and “Outstanding Contributions in International Achievement.”
Dr.Salas-Provance has served as a clinical educator throughout her academic career, especially related to children with cleft lip and palate. She is a member of an international medical team with Rotaplast International and has traveled worldwide for over 15 years to provide clinical services to children with cleft palate. She implemented a program for graduate students in speech pathology to provide clinical services in Spanish to children with cleft palate in Lima, Peru. In addition to Lima, Peru she has provided clinical services in China, Bangladesh, Philippines, El Salvador, Dominican Republic, Guatemala and Venezuela.
Dr. Salas-Provance is coauthor of the textbook Culturally Responsive Practices in Speech-Language and Hearing Science (Plural Publishing, 2019) which meets the needs for training students in healthcare professions regarding practice with individuals from culturally and linguistically diverse populations. Her research is focused on attitudes towards disability by diverse populations and addressing the use of language interpreters during healthcare and educational encounters.
Over the past ten years she has lectured extensively to international audiences, both in English and Spanish, including as invited speaker for the Congreso Internacional en Trastornos de la Comunicacion at Escuela de Fonoaudiologia (Speech Language Pathology / Audiology) de la Universidad de Talca, Chile and for the Department of Otolaryngology, Hospital Nacional Arzobispo Loayza, Lima, Peru, Endoscopic Evaluation of Velopharyngeal Dysfunction. She was invited keynote speaker for the First International Congress in Speech-Language Pathology and Orthodontics in the area of cleft lip and palate in Lima, Peru.
Dr. Salas-Provance was selected for the American Council on Education (ACE) Women’s Leadership Program and attended the National Women’s Leadership Forum in Washington DC (2017) for advancing female executives in higher education.

Kaylynn Schmitt is the Program Manager for the Department of Athletic Training. Mrs. Schmitt brings over 10 years of administrative and clerical experience to our program, working closely with the Department Chair, Program Director, and faculty with administrative responsibilities for both the Doctor in Athletic Training and Master in Athletic Training programs.

Valerie Hill began working at A. T. Still University in December 2022 as the Administrative Assistant for the Department of Interdisciplinary Health Sciences and the Department of Athletic training. Valerie joined ATSU’s team with over 30 years of administrative experience from another local institution of higher education.
University Catalog
 Read the University Catalog to learn more about the Doctor of Athletic Training online program and university.
Read the University Catalog to learn more about the Doctor of Athletic Training online program and university.
Visit About Us to learn more about ATSU.
Accreditation
A.T. Still University is accredited by the Higher Learning Commission
230 S. LaSalle Street, Suite 7-500,
Chicago, IL 60604
Phone: 800.621.7440 | Fax: 312.263.7462
Email: info@hlcommission.org
Degree-granting authority for the Arizona School of Health Sciences has been given by the Arizona State Board for Private Postsecondary Education, 1400 West Washington Rd., Room 260, Phoenix, AZ 85007. Phone 602.542.5709.
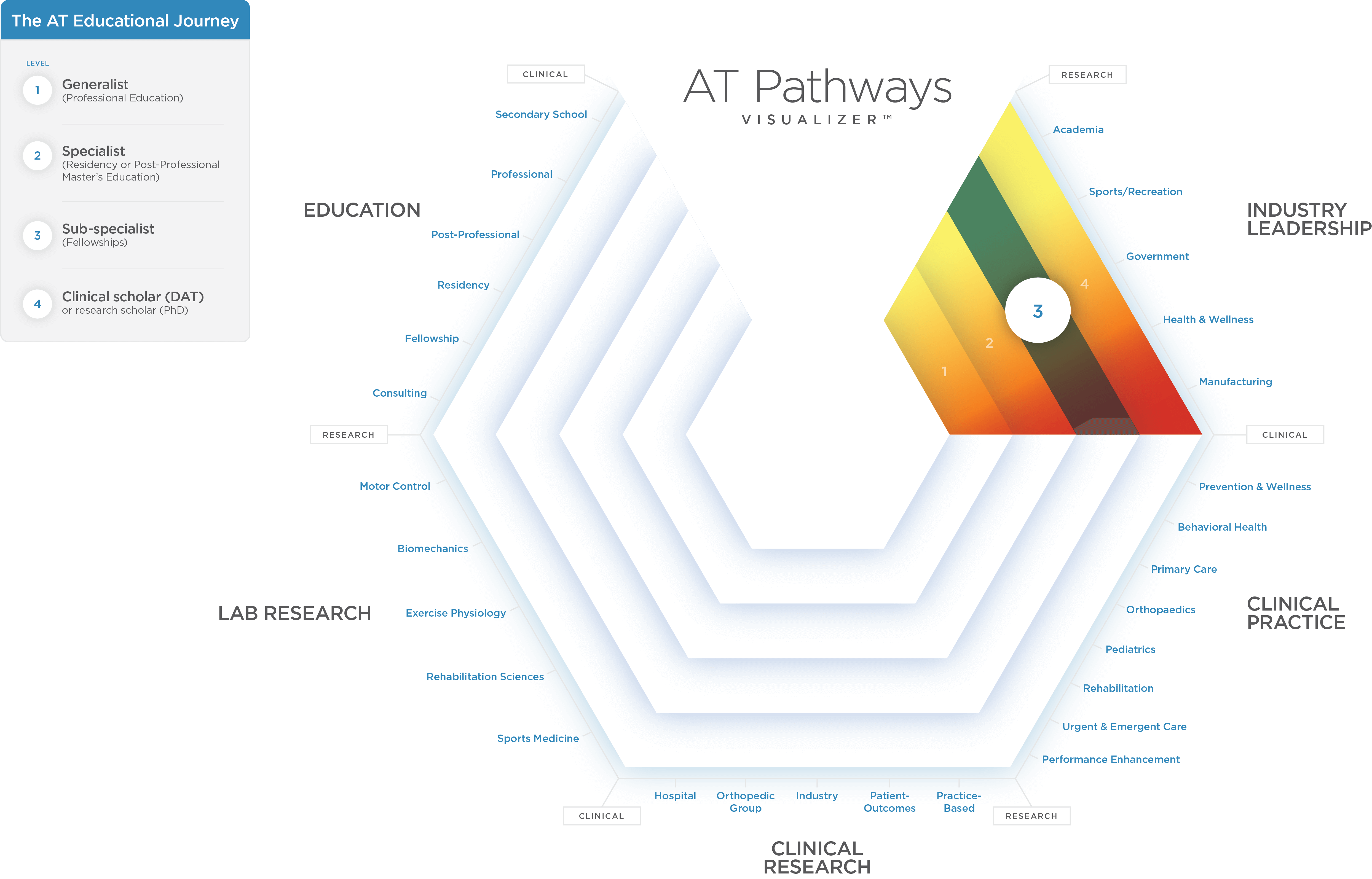
Educational pathways and professional opportunities
With so many educational options and different opportunities within athletic training curricula, the first step is matching your desired professional outcomes to the right educational tracks.
Click on the graphic below to start exploring.
Why Graduate Certificates in AT?
Do you want to focus on your passion points and areas of interest? Then, our AT graduate certificate programs offer a way to do just that. If you want a terminal degree, then use these to build a clinically-focused athletic training doctoral degree.
READ MOREPhD vs. Doctorate in Athletic Training?
Love doing lab research or want a generic terminal degree? Or, do you want a clinically-focused terminal AT degree with an emphasis on teaching the next generation of practitioners, conducting research in the field, or becoming the AT expert at the point of care?
READ MOREDoctor of Athletic Training program administration and faculty
Sports medicine leadership and expertise is demonstrated throughout the program, including by ATSU’s faculty and staff. Renowned faculty are recognized experts with national influence who share emerging trends and opportunities in athletic training practice and education. Interaction with a variety of instructors offers students exposure to a variety of teaching styles, healthcare- and education-related backgrounds and experiences that contribute to a well-rounded education fostering personal and professional growth.
Doctor of athletic training research
The Athletic Training program seeks to foster the value of scholarly activity and to develop students’ leadership skills in the research aspects of athletic training. The multidisciplinary setting at ATSU-ASHS, which includes physical therapy, occupational therapy, physician assistant studies, and audiology, promotes cross-disciplinary scholarship and provides students with exposure to a variety of different research programs.
Research
The Interdisciplinary Research Laboratory is a 3,000 square-foot facility with an expanded offering of research equipment and opportunities to study neuromuscular, metabolic, and cognitive function.
The Interdisciplinary Research Laboratory houses and supports equipment to study neuromuscular and cognitive function, including:
- 12-camera Vicon™ Motion Analysis System with Motion Monitor™ software and high-performance computer to capture kinematic data
- EMG unit, the Noraxon Wireless TeleMyo DTS 16-channel system, for assessment of neuromuscular performance characteristics
- In-floor Kistler 9286 AA Slimline Force Plate, a portable multi-component force plate for measuring ground reaction forces and moments acting in any direction
- GaitRite gait analysis system
- NeuroCom Smart Balance Master with a long forceplate and the Dynavision system, for measuring postural stability and vestibular function
- RealEyes™ binocular XDVR video goggles and camera for assessing and recording eye movements
- LigMaster computerized stress device, available for assessment of ankle, knee, elbow, and glenohumeral joint force-displacement characteristics
- MiniSim™ driving simulator system with Logitech™ G27 steering wheel/pedals/shifter and instrument button boxes for control of equipment (i.e., wipers, light, mirrors) that interfaces with a high-performance computer with high speed graphics card and three 24” monitors with software for MiniSim™ driving simulator system
- 2 GE LOGIQ e diagnostic ultrasound units
- 4 desktop and laptop computers dedicated to data analysis and writing
- Custom made joint stiffness device
- Electrogoniometers, accelerometers, and hand-held dynamometers
The Interdisciplinary Research Laboratory also houses and supports equipment to study exercise and metabolic function, including:
- Parvo metabolic system with ECG
- CosMed portable metabolic system
- Treadmill
- Lode electronically braked adult and pediatric cycle ergometers
- Monark cycle ergometer
ATSU’s Mesa Campus Learning Resource Center (LRC) supports the teaching and eventual practice of students and the teaching and research of its faculty. The LRC takes advantage of electronically based information resources that have developed since the emergence of the Internet a decade ago to facilitate and support access and use evidence in support of all instruction, research, and services at the University. The LRC’s collections are a blending of print and electronic resources to bring information access into the curriculum and clinical rotations of the students.
Access to and use of the LRC’s electronic resources is facilitated through its website (on the ATSU Intranet) and its online portal. The web site provides access to the LRC’s print holding, information on services provided and copies of LRC service request forms. The portal provides access to, and facilitates use of, more than 1,000 clinically oriented electronic, full text journals, more than120 full text medical textbooks, and an array of web-based, health information-based vendors. Via the LRC’s membership in the National Network of Medical Libraries’ Docline interlibrary loan system and OCLC’s interlibrary loan system, it can rapidly borrow books and articles from more than 20,000 libraries worldwide. More than 75 percent of the articles obtained from other libraries are received digitally within three days.
DAT Applied Research Project (ARP)
The goal of the Applied Research Project (ARP) is to advance practical knowledge in athletic training based on applied research and analysis. Students will identify a project of interest that is applicable to their work setting and learn the process of identifying a problem, researching solutions, implementing change, and measuring outcomes. The ARP may not always result in a publishable manuscript, but should provide the student with an understanding of the quality improvement and/or research process.
Students in the DAT have three primary options to complete their ARP requirements, the quality improvement option, case study option, or the original research option. Each option will follow the progression of the four ARP courses and culminate in an ARP presentation and written paper.
Quality improvement projects
To view completed applied research projects, please visit our ARP Showcases (https://my.ltb.io/#/showcase/atsudat)
Faculty research interests
Dr. Anderson’s primary research interests are focused on assessment of fundamental movement patterns and application of corrective exercise in orthopaedic rehabilitation. He has expertise in use of the Functional Movement Screen (FMS) and Selective Functional Movement Assessment (SFMA) and is currently involved in research looking at the use of the FMS in injury risk prediction and corrective exercise interventions. In addition, he also has research interests in post-professional clinical education. Dr. Anderson is actively engaged in the continued development and maintenance of the CORE-AT Electronic Medical Record and has interests in its application in clinical education.
Dr. Welch Bacon has methodological expertise in survey and qualitative research design. Her research interests include athletic training educational outcomes, with a specific focus on the incorporation of healthcare competencies within athletic training education, identifying effective educational techniques to aid athletic trainers in learning the fundamentals of evidence-based practice, competency-based education, and knowledge translation models.
Dr. Falsone’s research interests include the effects of dry needling on orthopedic rehab and sport performance as well as cupping and its effects on blood flow, tissue decompression and stiffness. She is also interested in breathing assessment and interventions and upper extremity rehabilitation and sport performance techniques.
Dr. Lam’s current line of research seeks to understand the overall impact of sport-related lower extremity injuries on patient-oriented outcomes. Specifically, Dr. Lam is interested in identifying the immediate and long-term impact of ankle and knee injuries on patient outcomes such as self-report of function and health-related quality of life. Through his research, he hopes to gain a better understanding of the patient’s perspective with the aim of improving patient outcomes and quality of care following a sport-related injury. To that end, Dr. Lam’s research interests also include identifying new methodologies to support comparative effectiveness research in sports medicine including the use of practice-based research networks, point-of-care clinical trials, Bayesian statistics, and healthcare information technology (eg, electronic medical records, big data, mobile devices).
Dr. McLeod’s ongoing line of research revolves around sports medicine concerns of the pediatric athlete, with special emphasis on sport-related concussion. Dr. McLeod completed her dissertation on the use of clinical assessment tools for concussion in youth sports athletes. She has also looked at factors affecting the use of clinical concussion assessments such as practice effects and exertion and sat on the NATA Pronouncements Committee on the Management of Sports Related Concussions. Her current work is investigating the short- and long-term effects of pediatric sports concussion as well as recovery following concussion on traditional concussion measures and health-related quality of life and concussion awareness and education among various healthcare providers and school personnel. Dr. McLeod also has research interests regarding appropriate medical care for secondary school and collegiate athletics.
Dr. Valier’s research focuses on clinical outcomes assessment, with an emphasis on the evaluation of health-related quality of life (HRQOL). Her primary area of interest is in evaluating the HRQOL of high school and college athletes who suffer sport-related injury. She has investigated HRQOL in adolescent athletes in both the secondary school setting as well as in outpatient orthopaedic clinics. Dr. Valier is also interested in the use and development of patient-reported outcomes instruments for the purpose of outcomes assessment and measuring the end result of healthcare services. Her interests also include the measurement properties and interpretation of patient-reported outcome measures, with special attention towards meaningful change values (eg, minimal clinically important difference and minimal detectible change) and instrument interpretation. In addition to her concentration in clinical outcomes assessment, Dr. Valier’s research interests include epidemiology and better understanding risks and rates of sport-related injury as well as healthcare quality improvement methodologies for optimizing athletic training systems of care.
DAT student Applied Research Projects
Original research
Teresa Kikugawa, June 2018
Kyle Mohr, June 2018
Joni Davenport, June 2018
Alicia Belant, June 2018
Sarah Cayton, June 2018
Christopher Anderson, June 2018
Taryn Pennington, June 2018
Stuart Wright, June 2018
Greg Janik, June 2018
Nicollete Stallworth Harris, December 2017
Greg Jancaitis, December 2017
Rebecca Ramirez McKinley, December 2017
Quinton Sawyer, December 2017
Nathan Slaughter, December 2017
Arika Cozzi, June 2017
Brandon Holland, June 2017
Kimberly Mace, June 2017
Garry Himes, June 2017
Lindsey Shepherd, December 2016
Case reports
Savannah Bailey, June 2018
Research links
American Academy of Orthopaedic Surgeons
American College of Sports Medicine
American Journal of Sports Medicine
American Orthoapaedic Society for Sports Medicine
American Shoulder and Elbow Surgeons
American Sports Medicine Institute
Brain Injury Association
Cincinnati Sports medicine Research and Education Foundation
Journal of Athletic Training
NATA-Research and Education Foundation
National Institutes of Health
National Library of Medicine
National Science Foundation
Orthopaedic Research and Education Foundation
PUB-MED
The Aircast Foundation