Module 1
Learning Objectives:
Definitions:
Dental caries is the most prevalent childhood disease in the US and it is the most common cause of tooth loss for children and adolescents. One in five have untreated dental caries and about 75% have existing dental restorations. Dental caries disproportionately affects minorities and the disadvantaged.
Everyone has dental biofilm on their teeth. Not everyone gets dental caries. This module should help you see how the interaction between host factors, host behaviors, host diet, dental biofilm and plaque can result in dental caries.
Risk Factors for Dental Caries
Host factors
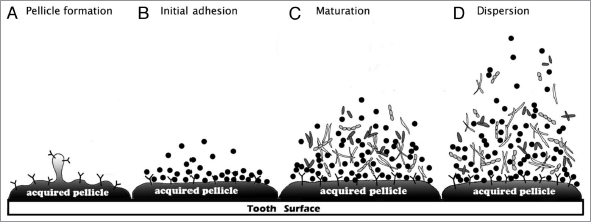
https://microbewiki.kenyon.edu/index.php/File:Dental_plaque_formation_wiki.png
A diverse collection of oral microorganisms are found in dental biofilms. A small sample of dental biofilm yields cultures containing between 12 and 27 bacterial species. After a thorough cleaning to remove dental biofilm on the tooth surface it only takes about 24 hours for dental biofilm to form again. If not removed by brushing two times a day and daily flossing the biofilm can accumulate to form plaque.
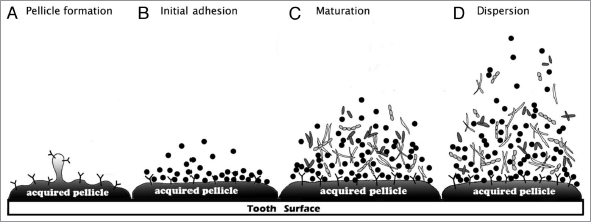
 |
Gram Stain of Dental Plaque https://microbewiki.kenyon.edu/index.php/File:20100926_180209_DentalPlaque.jpg |
A. Pellicle formation (Association)
Acquired Pellicle- Within seconds of tooth eruption, or after cleaning, tooth surfaces are coated with a conditioning film of molecules (e.g., biologically active proteins, glycoproteins) from saliva, gingival crevicular fluid, and from bacteria present in the oral cavity.
B. Initial adhesion (Adhesion and Proliferation)
Initial Adhesion- only a few bacterial species, the primary colonizers, attach to the acquired pellicle. Most of them are gram positive and include several Streptococcus species. Other primary colonizers include Actinomyces, Haemophilus, Neisseria and Veillonella. Cells are held reversibly near the tooth surface by weak, long-range physicochemical forces. Adhesins on these early bacterial colonizers, mainly streptococci (eg, Streptococcus mitis, S oralis, S. sanguinis and S. gordonii) can bind to complementary receptors in the acquired pellicle to make the attachment irreversible and allow the bacteria to multiply on the tooth surface. The metabolism of the primary colonizers changes the local environment on the surface of the tooth by making it more anaerobic.
Secondary colonizers- Adhesins on the cell surface of more fastidious secondary colonizers, such as obligate anaerobes, bind to receptors on already attached bacteria by coadhesion (binding together of an organism in suspension with an organism that has adhered to the tooth surface) or coaggregation (binding together of two organisms in suspension). The composition of the biofilm becomes more diverse (microbial succession). These secondary colonizers are mostly gram negative organisms and include Porphyromonas and Fusobacterium.
C. Maturation (Microcolony formation, Biofilm formation, and Maturation)
The bacterial colonizers produce extracellular polymers or extracellular polymeric substances (EPS) that consolidate attachment of the biofilm/plaque. EPS are usually polysaccharides (long chains of sugar/carbohydrates).
The biofilm/plaque EPS-
a. can bind to and retain molecules (enzymes)
b. can slow the penetration of charged molecules
c. provides the heterogeneous conditions within the biofilm that induces novel patterns of bacterial gene expression
d. allows the close proximity of different species resulting in microbe-to-microbe interactions
Microbe-to-microbe interactions include:
a. development of food chains (the end product of metabolism of one organism is used by secondary feeders);
b. metabolic cooperation among species to breakdown structurally complex host macromolecules;
c. cell-cell signaling by the secretion of small peptides to coordinate gene expression among cells of a species;
d. transfer of antibiotic resistance genes;
e. antagonism- production of inhibitory molecules giving the producing organisms competitive advantages within the biofilm. Production of molecules to exclude microbes that are detrimental to the inhabitants of the biofilm or the integrity of the biofilm.
The microbial composition of the biofilm varies depending of the site it attaches to on the tooth (e.g., fissures, approximal surfaces and gingival crevice).
The normal microflora of the biofilm on;
a. fissures is sparse and the organisms present have a saccharolytic metabolism (i.e., their energy is derived from sugar breakdown); the predominant bacteria are streptococci and there are few gram-negative or anaerobic organisms.
b. gingival crevices has a more diverse microflora, including many gram-negative anaerobic and proteolytic species
c. approximal surfaces has a microflora that is intermediate in composition between that seen in fissures and gingival crevices.
Once established, the composition of the resident microflora remains stable (microbial homeostasis). Normal pH in the environment around the organisms is about 7.0. The microflora in the dental biofilm will change if the environment changes. A major shift in the local environment can drive alterations in the microflora that can result in dental caries (dental biofilm gone bad= plaque).
D. Dispersion
Organisms leave the mature biofilm and are taken by the saliva to other teeth and surfaces in the mouth. The higher the number of cariogenic organisms in the saliva the higher the chances of dental caries developing underneath plague when it forms.
|
Top image- teeth before treatment with plaque-revealing gel Bottom image- teeth after treatment with plaque-revealing gel https://en.wikipedia.org/wiki/Dental_plaque#/media/File:Plaque_Disclosing_Gel.png |
How does dental biofilm go bad or become plaque? Or what increases the numbers of cariogenic bacterial in dental biofilm?
Dental biofilm + long time periods without removal of the biofilm + sucrose consumption + low pH = increase in biofilm mass and in cariogenic bacteria in the biofilm leading to plaque formation.
When more cariogenic bacteria are present in the plaque the pH remains at or below pH5.5 for longer periods of time resulting in demineralization of tooth enamel.
How biofilm goes bad (plaque) and can cause dental caries.
As biofilm grows it becomes thicker and visible upon inspection. Meanwhile, the consumption of sugar causes an environmental change in the dental biofilm microflora. Fermentation of sucrose results in lactic acid (lactate) production. Lactate lowers the pH of the dental biofilm. (Note: Table sugar is sucrose and sucrose is a disaccharide consisting of glucose and fructose; Biochemical moment; go ahead click the link; I dare you)
Cariogenic bacteria (Streptococcus mutans, S. sorbrinus and Lactobacillus casei) present in the dental biofilm increase in numbers compared to the rest of the organisms in the biofilm because they are acid-tolerant. If the dental biofilm enriched in cariogenic bacteria (plaque= dental biofilm gone bad) is allowed to remain for long periods of time and if the environment is rich in sugar the pH in the biofilm, now visible and called plaque, can go to pH 5.5 or lower.
At pH’s to or below 5.5 the tooth demineralizes and cavities can result. Cavity formation depends on how long and how frequently the pH goes to or below pH 5.5. If the times of low pH are short and infrequent, cavity production is less likely. If the times of low pH are long and frequent, cavity production is more likely.
If sugar intake stops, the pH of the plaque will rise and remineralization of the enamel occurs. Caries will result if the acidification-demineralization phase is more damaging and more frequent than the repair phase (alkalinization-remineralization phase).
What organisms are more likely to have cariogenic abilities?
Mutans group of Streptococcus; S. mutans and S. sobrinus
Lactobacillus casei, Actinomyces spp., Bifidobacterium spp., and low-pH tolerant Streptococcus spp.
Cariogenic bacterial species are present in healthy dental biofilm. There is not one particular bacterial species responsible for caries production, but a collection of several bacterial species that have the following abilities; acidogenicity, aciduricity, production of extracellular polymers and production of intracellular polysaccharides. When dental biofilm becomes visible and is enriched in cariogenic bacteria then this biofilm is called plaque and it can produce dental caries in a sucrose-rich environment.
Four microbial characteristics, or cariogenic abilities, are common in cariogenic bacterial inhabitants of dental plaque;
1. Acidogenicity- rapid uptake and fermentation of carbohydrates to lactic acid or other acidic byproducts
2. Aciduricity- the ability to tolerate, grow, and continue to make acid in acidic (low-pH) environments
3. Extracellular polymers- the synthesis of extracellular polymers or EPS from sucrose to consolidate attachment of the plaque to the surface of the tooth
4. Intracellular polysaccharides- the production of intracellular polysaccharides during periods of excess carbohydrate availability which can be converted to acid during times when carbohydrates are not available.
Timing of Plaque, Calculus and Dental Caries Formation
After a thorough cleaning to remove dental biofilm on the tooth surface it only takes about 24 hours for dental biofilm to form again. If not removed by brushing two times a day and daily flossing the biofilm can accumulate to form plaque. If the plaque is mineralized it becomes calculus (tartar). Plaque formation and its mineralization to calculus takes on average about 12 days (range of 10 to 20 days). Calculus is difficult to remove and REQUIRES professional cleaning to remove it. If plaque and calculus are not regularly removed patients are much more likely to develop dental caries and periodontal disease (See Dental Biofilm/Plaque; Bad to the Gums, Ligaments and Bone). Dental caries can develop within a few months or may make take years to develop.
Fissure Caries
Subgingival Caries
Prevention of Dental Caries
Test yourself to see what you have learned
References:
Dye BA, Li X, Beltrán-Aguilar ED. 2012. Selected oral health indicators in the United States, 2005–2008. NCHS data brief, no 96. Hyattsville, MD: National Center for Health Statistics. http://www.cdc.gov/nchs/products/databriefs/db96.htm
Marsh PD. 2010. Microbiology of Dental Plaque Biofilms and Their Role in Oral Health and Caries. Dent Clin N Am. 54:441-454. doi:10.1016/j.cden.2010.03.002
© 2016 Neal R. Chamberlain,Ph.D., and Priscilla L. Phillips, Ph.D. All rights reserved.
Site Last Revised 10/11/16
Neal Chamberlain, PhD. and Priscilla L. Phillips, Ph.D. A. T. Still University of Health Sciences/Kirksville College of Osteopathic Medicine.
Take Care and Think Microbiologically!
Disclaimer:
None of the contributors to this web site assume liability for any use or misuse of the information provided here. This information does not replace dental/medical consultation, but is intended for EDUCATIONAL purposes only. Any mention of commercial products is for inclusive purposes and is not an endorsement. Every effort has been made to provide accurate information about the products mentioned in this web site, but consult product labels for the most up-to-date information available. This web site does not constitute a medical diagnosis; seek advice from a dentist/physician (if you are not one yourself) before making a diagnosis and/or undertaking any of the treatments suggested here.