Previous Lecture | Syllabus | Next Lecture
2. To emphasize the eukaryotic nature of the fungi and its relationship to pathogenesis.
3. To establish familiarity with the scientific terminology peculiar to mycology.
4. To explore the nature of the pathogenesis of fungal infections.
5. To gain familiarity with the classification of medically-important fungi.
6. To develop an understanding of the nature and mode of action of anti-fungal agents.
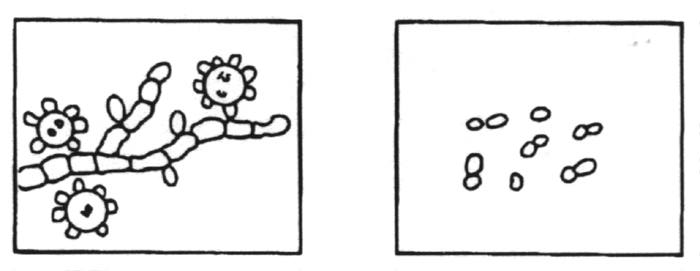
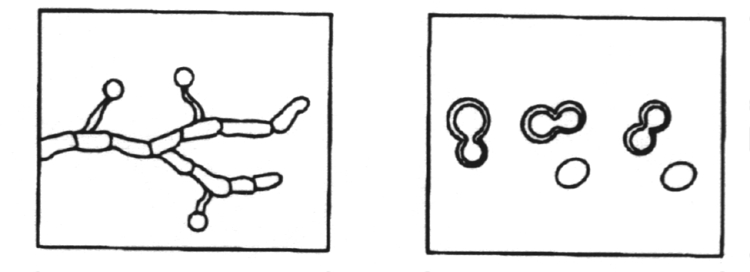
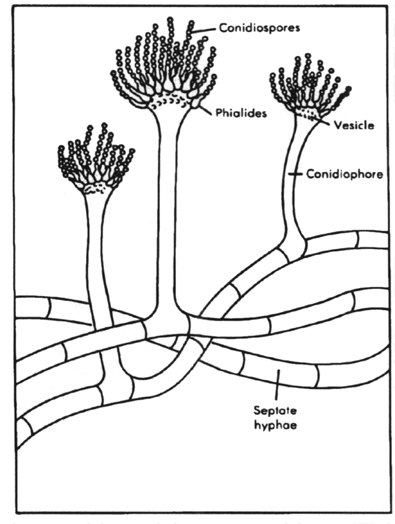
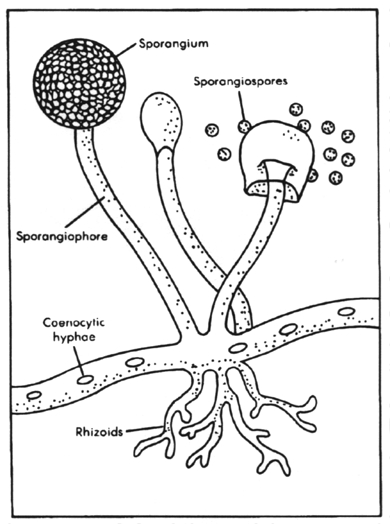
Fungi can be divided into two basic morphological forms, yeasts and hyphae. Yeastsare unicellular fungi which reproduce asexually by blastoconidia formation (budding) or fission. Hyphaeare multi-cellular fungi which reproduce asexually and/or sexually. Dimorphism is the condition where by a fungus can exhibit either the yeast form or the hyphal form, depending on growth conditions. Very few fungi exhibit dimorphism. Most fungi occur in the hyphae form as branching, threadlike tubular filaments. These filamentous structures either lack cross walls (coenocytic) or have cross walls (septate) depending on the species. In some cases septate hyphae develop clamp connections at the septa which connect the hyphal elements.
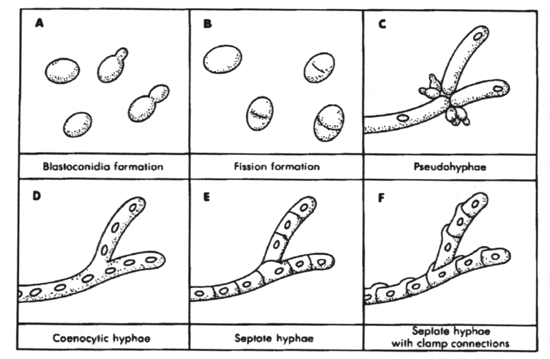
A.
Yeast cells reproducing by blastoconidia formation; B. Yeast dividing by
fission; C. Pseudohyphal development; D. Coenocytic hyphae; E. Septate
hyphae; F. Septate hyphae with clamp connections
From
Medical
Microbiology, 1990, Murray, et al., p. 299, Fig. 28-1. Reproduced with
permission.
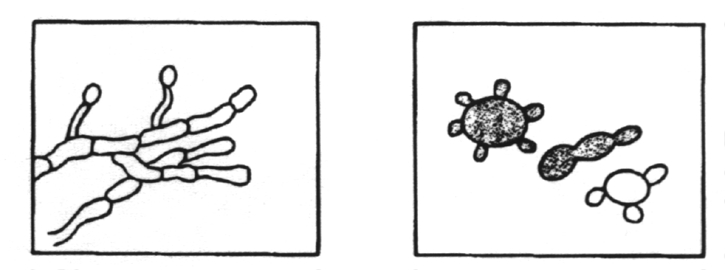
A mass of hyphal elements is termed the mycelium (synonymous with mold). Aerial hyphae often produce asexual reproduction propagules termed conidia(synonymous with spores). Relatively large and complex conidia are termed macroconidia while the smaller and more simple conidia are termed microconidia. When the conidia are enclosed in a sac (the sporangium), they are called endospores. The presence/absence of conidia and their size, shape and location are major features used in the laboratory to identify the species of fungus in clinical specimens.
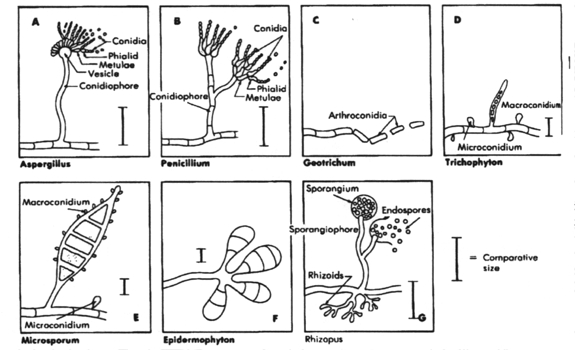
A. Aspergillus; B. Penicillium; C. Geotrichum; D. Trichophyton; E. Microsporum; F. Epidermophyton and G. Rhizopus. From Medical Microbiology, 1990, Murray, et al., p. 300, Fig. 28-2. Reproduced with permission.
Asexual reproduction, via conidia formation, does not involve genetic recombination between two sexual types whereas sexual reproduction does involve genetic recombination between two sexual types.
1. The
synthesis of chitin, a polymer of N-acetyl glucosamine, and other compounds,
for use in forming the cell wall. These
induce immune hypersensitivity.
2. The
synthesis of ergosterol for incorporation into the plasma membrane. This
makes the plasma membrane sensitive to those
antimicrobial agents which either block the synthesis of ergosterol or
prevent its incorporation into the membrane or bind to it,
e.g. amphotericin B.
3. The synthesis of toxins such as
a. Ergot alkaloids- these are produced by Claviceps purpurea and cause an alpha adrenergic blockade
b. Psychotropic agents - these include psilocybin, psilocin and lysergic acid diethylamide (LSD)
c. Aflatoxins
- these are carcinogens produced by Aspergillus flavus when growing
on grain. When these grains are eaten
by humans or when they are fed to dairy cattle and they get into the milk
supply, they affect humans.
4. The
synthesis of proteins on ribosomes that are different from those found
in bacteria. This makes the fungi immune to those
antimicrobial agents that are directed against the bacterial ribosome,
e.g., chloramphenicol.
5. The
ability of certain metabolites to alter morphology of yeast and/or be assimilated
by yeast with concomitant clinical
identification affects.
2. Positive stain with
3. Negative stain with India inkC. Culture of fungi on
2. Mycosel agar (selective for pathogenic fungi because of chloramphenicol and cycloheximide in medium)
2. Cellular
morphology
2. Behavior in broth and serum (germ tube formation)
3. Behavior on cornmeal agar (pseudohyphae formation)
Fatty acid content of the
skin
pH of the skin, mucosal
surfaces and body fluids
Epithelial turnover
Normal flora
Transferrin
Cilia of respiratory tract
When fungi do pass the resistance barriers of the human body and establish infections, the infections are classified according to the tissue levels initially colonized.
A. Superficial
mycoses - infections limited to the outermost layers of the
skin and hair. The superficial mycoses are:
B. Cutaneous mycoses - infections that extend deeper into the epidermis, as well as invasive hair and nail diseases.
These diseases are restricted
to the keratinized layers of the skin, hair and nails. Unlike the superficial
mycoses, various cellular immune responses may be evoked, causing pathologic
changes in the host that may be expressed in the deeper layers of the skin.
The agents causing these diseases are termed dermatophytes.
The diseases are referred to as ringwormor tinea.
All of the dermatophytic diseases are caused by members of three genera,
Microsporum,
Trichophyton and Epidermophyton, which comprise 41 species.
The cutaneous mycoses are:
C. Subcutaneous mycoses - infections involving the dermis, subcutaneous tissues, muscle and fascia
These infections initially involve the deeper layers of the dermis, subcutaneous
tissue or bone. Most infections have a chronic
or insidious growth pattern, eventually extending into the epidermis and
are expressed clinically as lesions on the skin
surface. They are initiated by trauma to the skin and are difficult to
treat and surgical intervention (excision or amputation)
is frequently employed. The subcutaneous mycoses are:
D. Systemic mycoses - infections that originate primarily in the lung and may spread to many organ systems.
Unlike most other fungi, the five systemic mycotic agents are inherently
virulent. Each species has biochemical and structural
features that enable it to evade host defenses. The primary focus of infection
is the lung but secondary infection may occur
elsewhere in the body. The five etiological agents are identified by their
morphology on agar plates (saprobic phase) and in
tissue (parasitic phase):
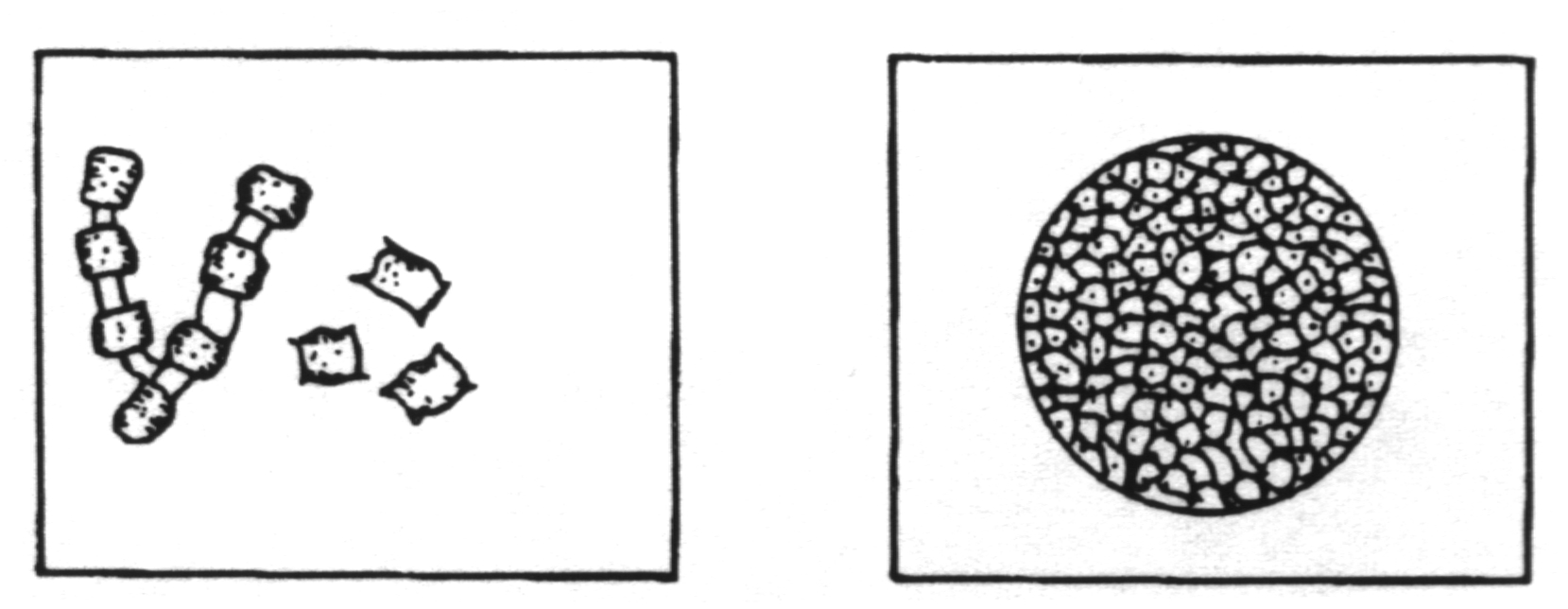
Dimorphic with mold to yeast transition when infecting susceptible species.
Yeast cells are relatively small. Saprobic phase
shows tuberculate macroconidia.
Dimorphic with mold to yeast transition when infecting susceptible species. Yeast cells are medium size with thick walls.
Dimorphic with mold to yeast transition when infecting susceptible species. Yeast cells have multiple buds.
Dimorphic with mold to spherule transition when infecting susceptible species. Spherules are multinucleate.
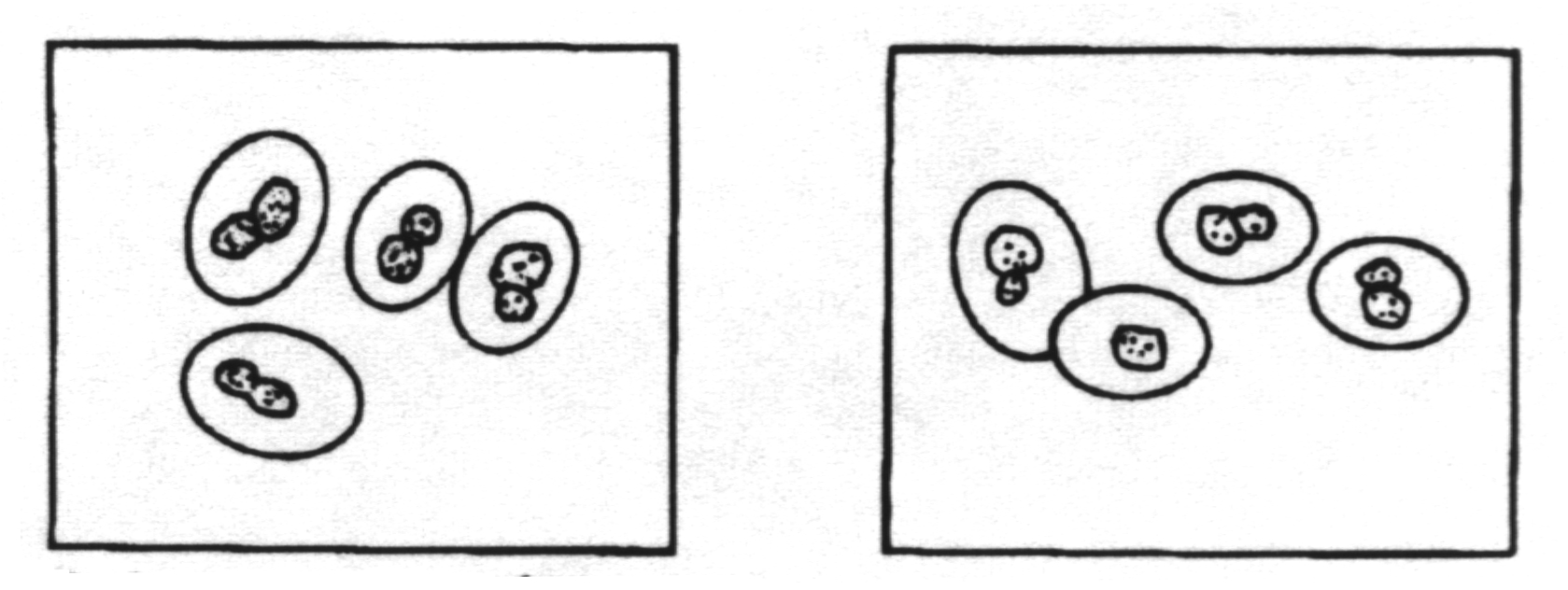
Monomorphic with yeast phase only. This is the only pathogenic yeast with a capsule. The capsule is extremely large.
E. Opportunistic mycoses - infections in patients with immune deficiencies who would otherwise not be infected
Opportunistic mycoses are seen in those people with impaired host defenses
such as occurs in
The major opportunistic mycoses
include:
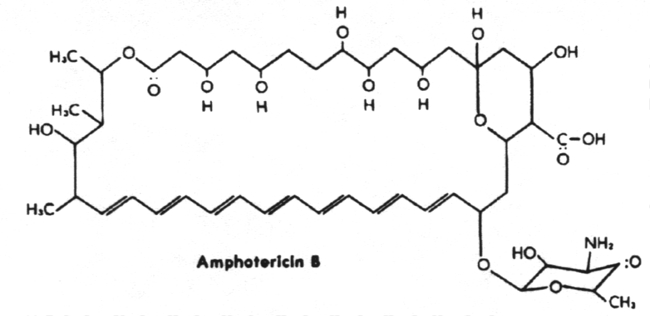
Nystatin - binds to ergosterol and disrupts plasma membrane. Highly insoluble and toxic and therefore used topically only.
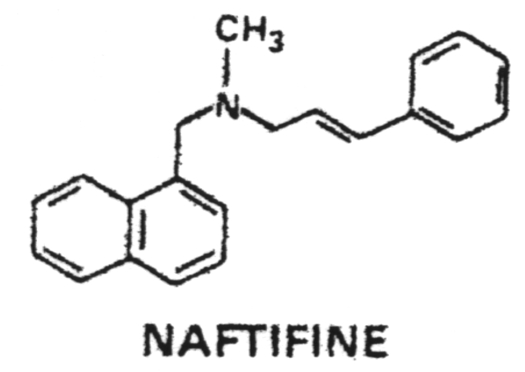
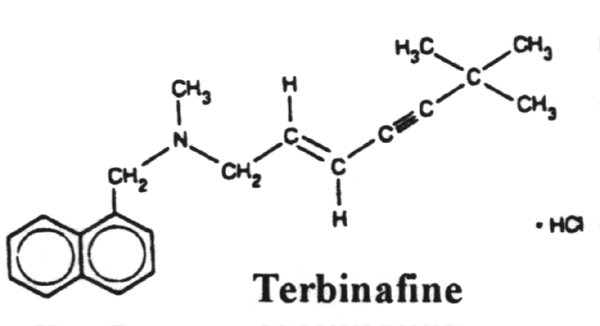
Terbinafine - Binds to and inhibits squalene epoxidase which blocks ergosterol synthesis.
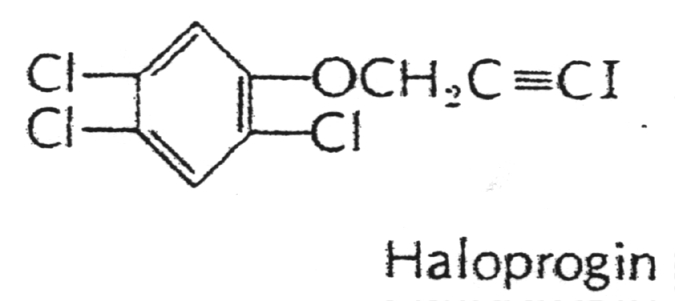
Haloprogin - a halogenated phenolic ether administered topically for dermatophytic infections.
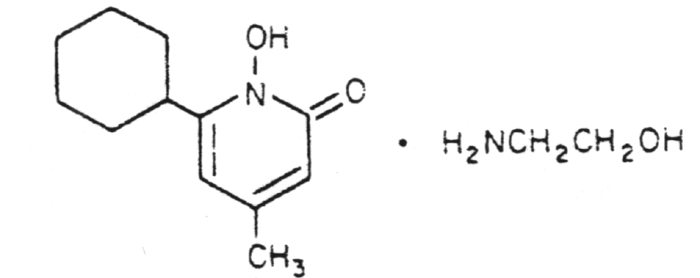
Ciclopirox olamine - a topical for the treatment of dermatophytic infections and Candida albicans.
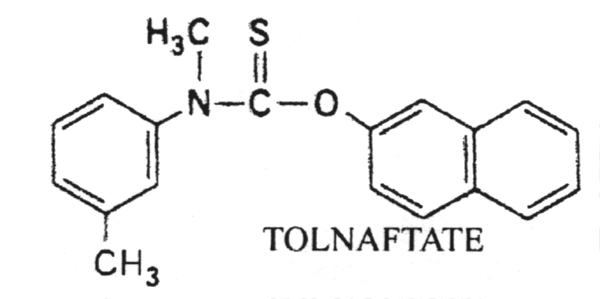
Tolnaftate - a thiocarbonate used to treat dermatophytic infections.
Potassium iodide (KI) - Given orally for sporotrichosis
2. Hyphae are branching, threadlike, tubular filaments that either lack cross walls (coenocytic) or have cross walls (septate).
3. Hyphae reproduce asexually via the formation of spores termed microconidia or macroconidia.
4. Fungi produce toxins such as ergot alkaloids, psychotropic agents and aflatoxins.
5. Visualization
of fungi in human tissue is accomplished by treatment with 10% KOH and
staining with lactophenol cotton blue,
Grocott silver stain, hematoxylin or eosin.
6. India ink may be used as a negative stain to emphasize the capsule of yeast.
7. The
physician can use an ultraviolet lamp (Wood's lamp) to detect fluorescent
compounds produced by fungi growing in or on
human tissue.
8. Fungal
diseases are classified according to their depth of penetration of human
tissue. Thus, there are the superficial mycoses,
cutaneous mycoses, subcutaneous mycoses and systemic mycoses.
9. The superficial mycoses include pityriasis versicolor, tinea nigra, black piedra and white piedra.
10. The cutaneous mycoses (tineas or ringworms) are restricted to growth in the keratinized layers of the skin, hair and nails.
11. The
subcutaneous mycoses penetrate the dermis, subcutaneous tissue, muscle
and fascia. These include sporotrichosis,
chromoblastomycosis and mycetoma.
12. Systemic
mycoses originate in the lung and then may spread to many organ systems.
These include histoplasmosis, North
American blastomycosis, South American blastomycosis, coccidioidomycosis
and fungal meningitis.
13. Fungi are most commonly cultured on Sabouraud's agar or Mycosel agar.
14. Opportunistic
mycoses are often secondary to other diseases that compromise host immunity
such as AIDS, diabetes, and
malignancy.
15. Antifungal
agents are classified according to their chemical structure as macrolides,
azoles, allylamines, pyrimidine analogs
and miscellaneous.
16. The polyene antifungals are amphotericin B and nystatin which bind to ergosterol in the plasma membrane, thus disrupting it.
17. The
azole antifungals include fluconazole and ketoconazole plus numerous others.
They all block ergosterol synthesis by
binding to cytochrome P-450.
18. The allylamines include naftifine and terbinafine which inhibit squalene epoxidase, thus blocking ergosterol synthesis.
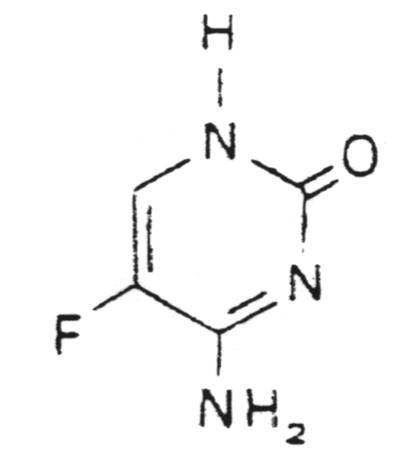
19. The
pyrimidine analogs such as flucytosine incorporate into RNA and/or DNA
thus blocking protein synthesis or DNA
synthesis.
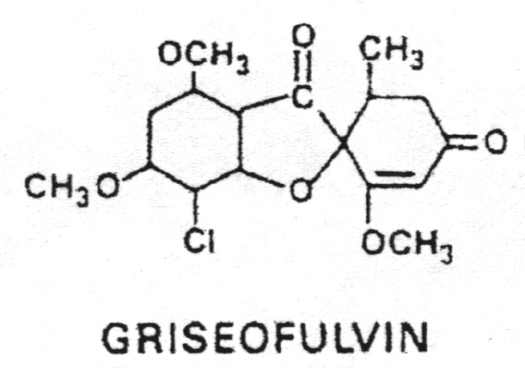
20. The miscellaneous antifungals include griseofulvin, haloprogin, ciclopirox olamine, tolnaftate and potassium iodide.
21. The three genera of dermatophytes are Microsporum, Trichophyton and Epidermophyton.